Oligotrophic Distal Femur Nonunion and Hardware Failure - Double Plate Septic Revision
Score and Comment on this Case
Clinical Details
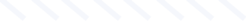
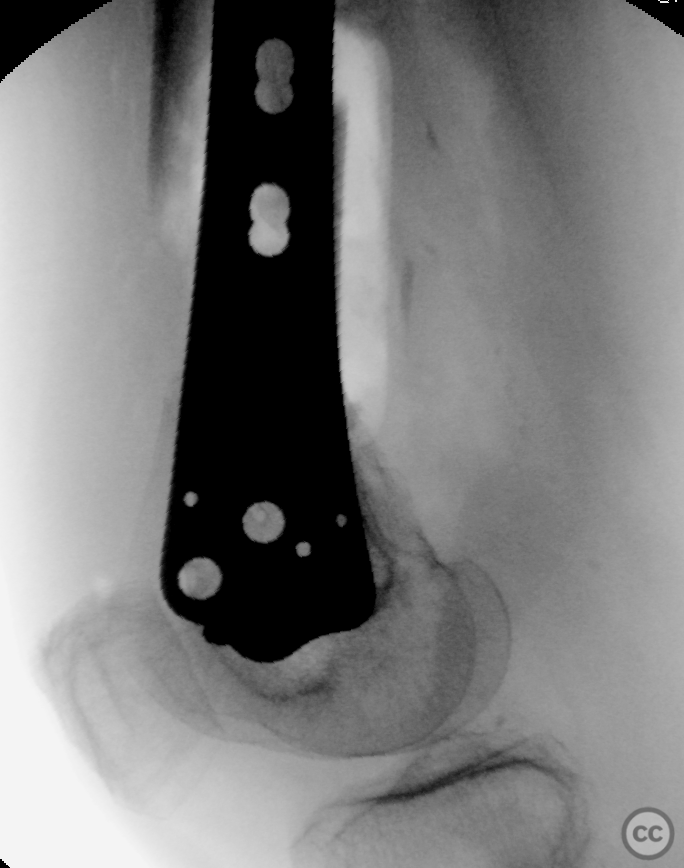
Clinical and radiological findings: An 86-year-old female with dementia, residing in a nursing home and previously independently mobile, presented with a distal femur fracture. Initial management involved lateral LISS plate fixation. Intra- and postoperative evaluation revealed significant bone defect, questionable bone contact and a leg length discrepancy of approximately 40mm. Followup radiographs at 6 months demonstrated hardware failure, characterized by breakage of distal screws and significant osteolysis around screw holes, and a fluffy oligotrophic nonunion atleast suggestive of a septic process.
Preoperative Plan
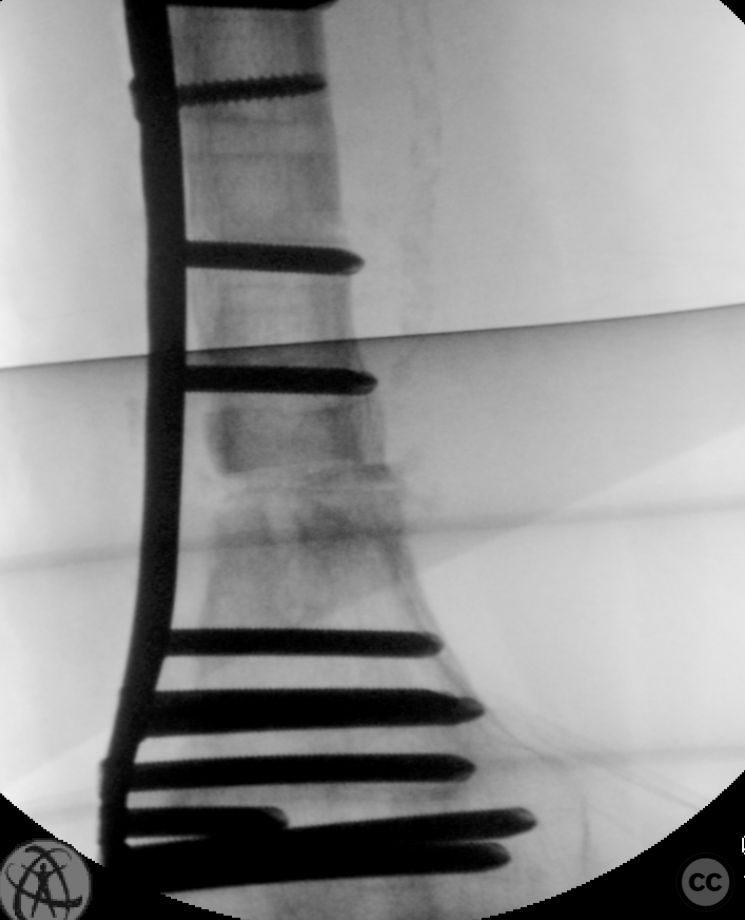
Planning remarks: The preoperative plan included staged revision due to concerns of septic nonunion. Initial debridement was to be followed by revision osteosynthesis. All samples taken from bone/fracture sample 1 sterile sample 2 sterile sample 3: low count Staphylococcus epidermidis sample 3: low count Micrococcus luteus sample 3: low count Propionibacterium acnes A second debridement yielded sterile results. Planing the definitive fixation, given the patient's short stature and existing hip prosthesis, a nail plate combination was considered but deemed unsuitable. The decision was made for double plate osteosynthesis with acute shortening and debridement.
Surgical Discussion
Patient positioning: The patient was positioned supine on the operating table with the affected leg positioned over a carbon fiber roll, allowing access to both the lateral and medial aspects of the distal femur.
Anatomical surgical approach: The initial approach involved a longitudinal incision along the lateral aspect of the right femur, utilizing the previous surgical scar for access. A vastus lateralis muscle-splitting approach was employed for lateral exposure. For medial access, a subvastus medialis approach was chosen, with an incision overlying the medial femoral condyle.
Operative remarks:During surgery, old hardware was removed, and debridement of the pseudarthrosis site was performed. An osteotomy with resection of approximately 15mm was executed to achieve healthy bone margins. An 11-hole femoral LCP was used for lateral stabilization, and a proximal lateral large fragment tibial locking plate was placed medially for additional support. Both plates were secured with locking screws under fluoroscopic guidance. Vancomycin powder was applied topically to the nonunion sites before closure.
Postoperative protocol: Postoperatively, no orthosis was applied; partial weight-bearing up to 50% body weight was allowed during recovery.
Follow up: Not specified
Orthopaedic implants used: Implants used included an 11-hole femoral LCP, proximal lateral large fragment tibial locking plate.
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisNonunion rates vary across studies but are generally considered modest when using lateral locked plating (LLP) techniques [1][2]. However, several factors have been identified that increase the risk of nonunion including high-energy fractures, intra-articular involvement, poor bone quality, severe comminution or bone loss [1], younger age groups [2], and specific mechanical construct characteristics related to overall rigidity [3].
The development of LLP has improved outcomes for distal femur fractures; however, there remains a subset of patients who experience nonunion despite these advancements [1]. In particular, Rodriguez et al. (2016) highlighted that certain construct characteristics associated with LLP fixation—specifically plate design/material—significantly influence the risk of nonunion independent of other variables such as number of proximal screws or plate length [3]. They found that stainless steel constructs had a higher rate of nonunion compared to titanium constructs (41% vs. 10%) indicating material properties play an essential role in fracture healing dynamics under LLP fixation strategies.
Wenger and Andersson's retrospective study on 191 consecutive patients treated with LLP revealed an overall low rate of nonunion at 4%, suggesting that when applied correctly and considering patient-specific factors such as age and open versus closed fracture status; LLP can be highly effective in achieving fracture union [2]. This study also noted younger patients had higher reoperation rates not directly correlated with nonunion but potentially indicative of more complex initial injuries or higher functional demands leading to complications.
On the other hand, dual plating (DP) techniques involving both medial and lateral plates have emerged as an alternative strategy purportedly offering biomechanical advantages over single lateral plating especially in cases with significant comminution or instability [1]. O'Neill et al.'s systematic review supports this notion by demonstrating favorable outcomes associated with DP including acceptable complication rates alongside good functional recovery metrics compared against previously published data on LLP alone [1].
In summary, while LP offers substantial benefits for managing distal femoral fractures concerning reducing the incidence of nonunion among other complications; individual patient factors along with specific surgical technique nuances significantly impact success rates. Evidence suggests utilizing materials like titanium over stainless steel may reduce risks inherently tied to construct rigidity under LLP modalities. Moreover, exploring DP options could further mitigate nonunion risks particularly within challenging clinical scenarios characterized by extensive bone damage or compromised stability.
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant
Industry Sponsership
contact us for advertising opportunities













Article viewed 897 times
08 May 2024
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2024). Oligotrophic Distal Femur Nonunion and Hardware Failure - Double Plate Septic Revision. Journal of Orthopaedic Surgery and Traumatology. Case Report 1295649 Published Online May 08 2024.