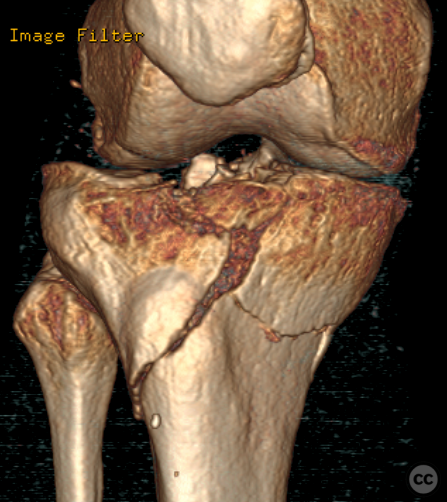
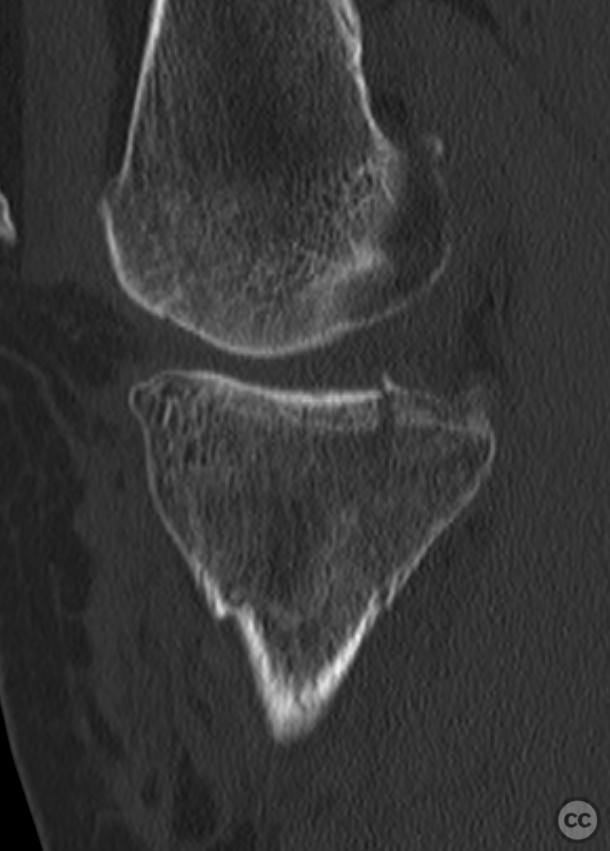
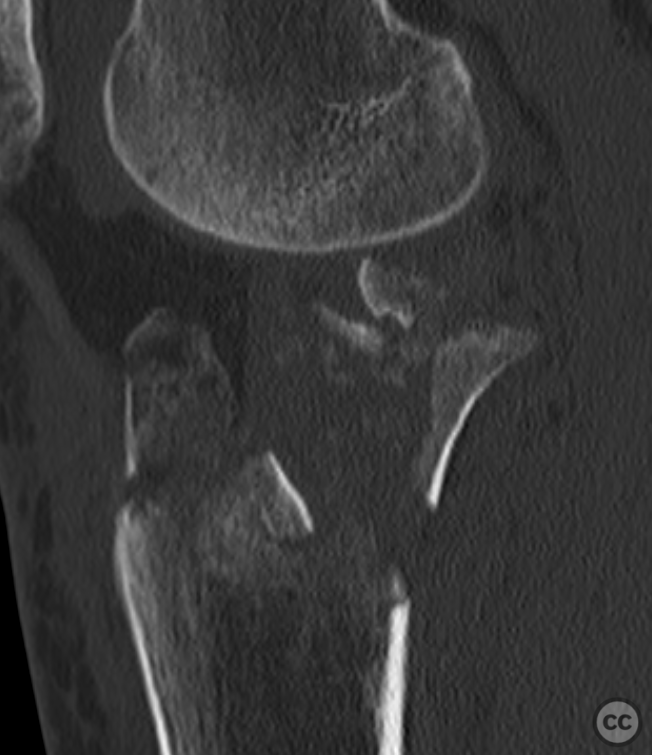
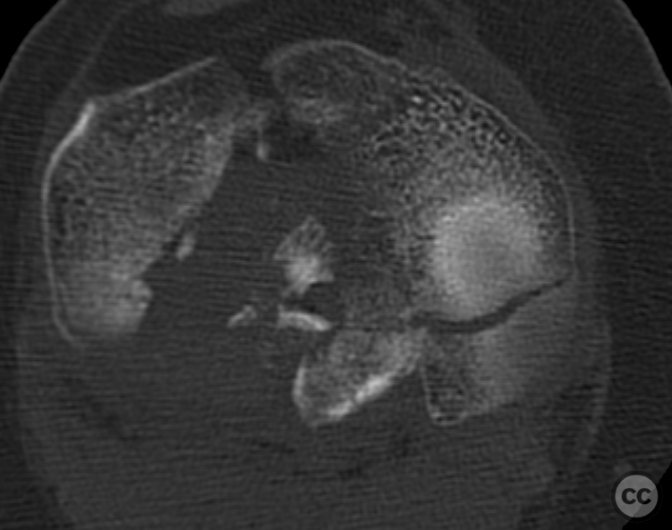
Schatzker VI tibial plateau fracture with ACL and meniscocapsular injury
Score and Comment on this Case
Clinical Details
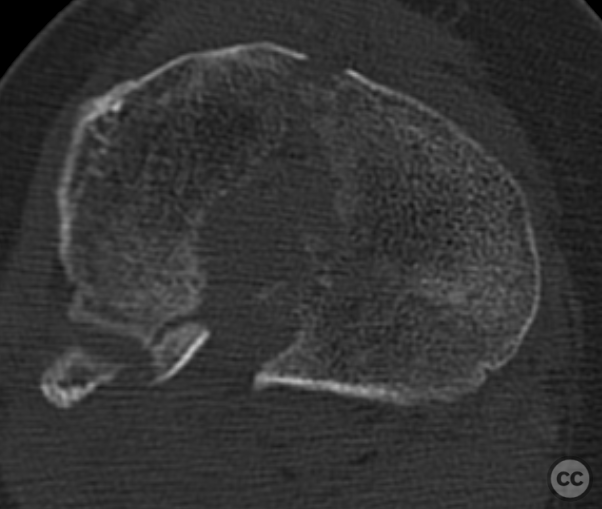
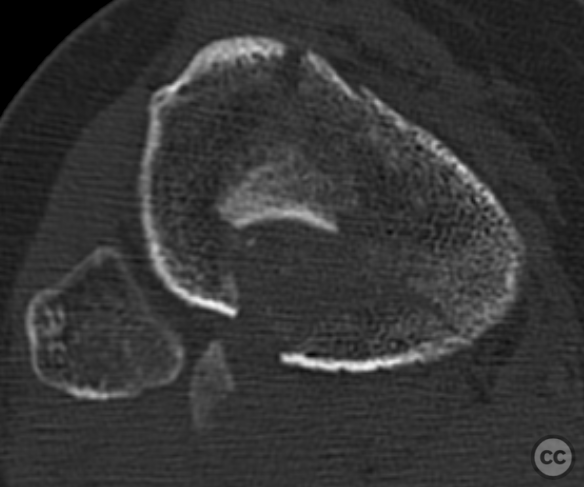
Clinical and radiological findings: A 62-year-old female presented with a right knee injury following a fall from a horse. Clinical examination revealed deformity, swelling, and an inability to bear weight. Plain film radiographs and CT confirmed a bicondylar Schatzker VI tibial plateau fracture (trending towards a Moore 2 fracture-dislocation) with minimal displacement of the medial column and simple articular split, alongside massive articular depression with central and posterolateral joint comminution on the lateral side.
Preoperative Plan
Planning remarks: The preoperative plan included addressing the medial column first due to its minimal displacement, using a medial approach for anatomic reconstruction. This would provide a stable medial column for subsequent repair of the more complex lateral injury. The lateral side would be approached through an anterolateral incision, with the goal of reconstructing the comminuted articular surface and addressing the subsequent meniscocapsular and ACL avulsion injurie.
Surgical Discussion
Patient positioning: The patient was positioned supine on a radiolucent operating table, with a carbon roll under the distal aspect of the right thigh to achieve approximately 30 degrees of knee flexion, allowing circumferential access to the proximal tibia.
Anatomical surgical approach: A longitudinal incision over the medial knee, followed by subcutaneous dissection and identification of the MCL and pes anserinus insertion. On the lateral side, a longitudinal incision over the lateral joint line, followed by identification and longitudinal splitting of the iliotibial band, with subperiosteal elevation from Gerdy's tubercle and distal extension into the fascia of the tibialis anteriormuscle.
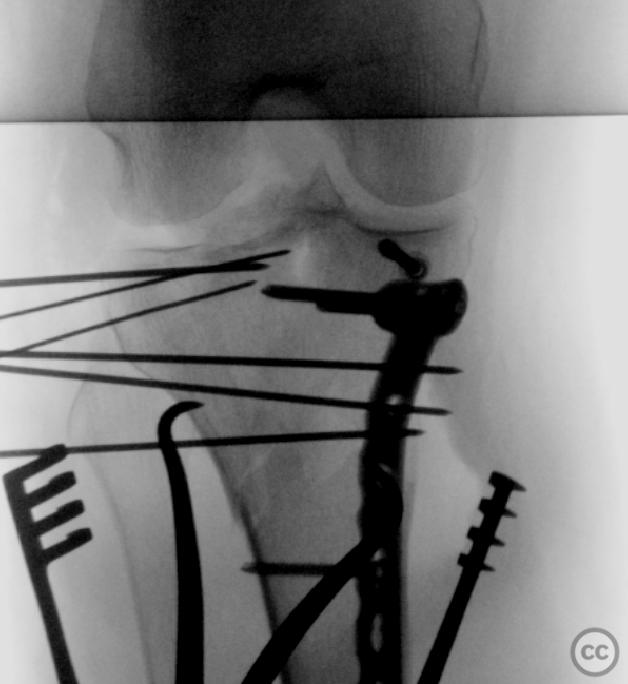
Operative remarks:Following the initial medial apporach, and prior to any further significant manipulation or reduction attempts, a K-wire was used to secure the non-displaced articular surface, followed by placement of a 4.0 mm cannulated screw parallel to the subchondral bone. This faciliateted mobilsation and reduction of the medial condyle enbloc. A proximal med. tibial locking plate was applied for column fixation.
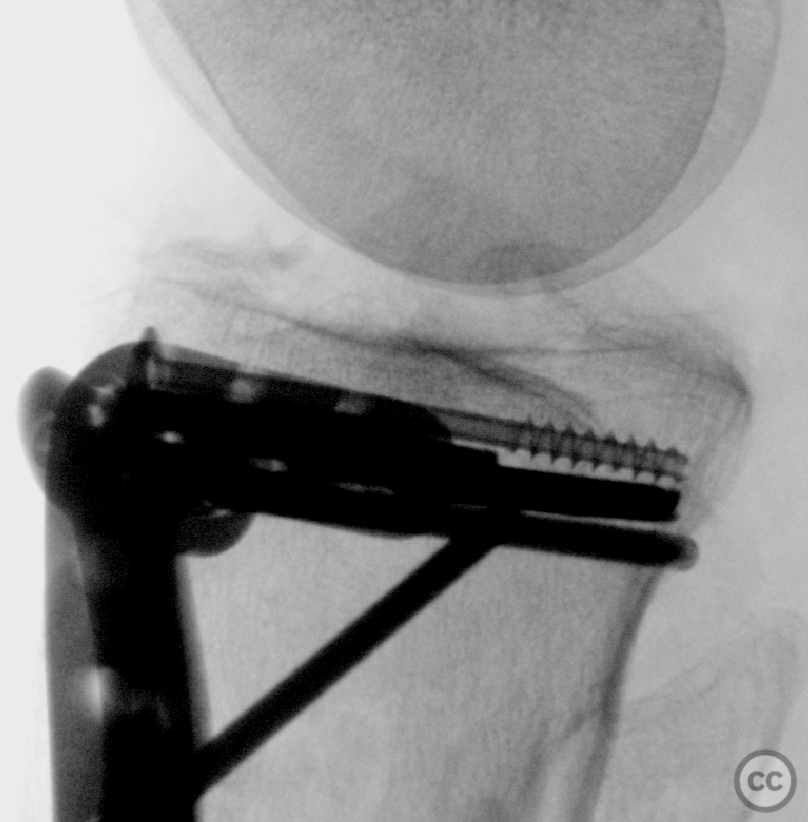
Laterally, after irrigation and debridement, a bucket handle tear (meniscocapsular separation) of the lateral meniscus was armed and mobilised with vicryl sutures. A bony avulsion of the anterior cruciate ligament from the intercondylar eminence was reduced and transfixed fixed with PLLA pins. The markedly depressed articular surface was mobilized and the the articular surface piece-meal reconstructed using K-wires in an inside-out fashion, followed by 'closing the door' and placement an anterolateral locking plate for definitive lateral column fixation.
The lateral eniscus was then secured to the postero- and anterolateral caspule, and additionally anchored to the anterolateral plate restoring radial tension and mensical function
Postoperative protocol: Postoperatively, an M4S knee orthosis was applied with an initial range of motion limited to 30 degrees of flexion. 2 year Follow, AROM 0-0-110deg, Normal domestic tasks including kneeing with minimal complaint. superfically palpable hardware was annoying, resulting in the patient undergoing elective removal of hardware
Orthopaedic implants used: 4.0 mm cannulated screws - Medial proximal tibial locking plate (3.5 mm, 8-hole) - Anterolateral locking plate (3.5 mm, 8-hole) - Vicryl sutures - Transfixation pins (PLLA) - Multiple K-wires
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisTibial plateau fractures are complex injuries often associated with concomitant soft-tissue damage [1,2]. Articular joint depression is a key parameter in evaluating these fractures on computed tomography (CT) scans. A consistent theme across the literature is that greater articular depression correlates with an increased risk of intra-articular soft tissue injuries such as meniscal tears [3-7], ligamentous disruptions [8], and subsequent development of posttraumatic osteoarthritis (OA) [1].
The degree of initial articular depression measured from preoperative CT scans has been shown to be a significant predictor for developing severe OA following medial tibial plateau fractures [1]. This suggests that the extent of chondral injury at the time of fracture may influence long-term joint health outcomes.
Moreover, lateral tibial plateau fracture depression has been linked to lateral meniscus pathology. Specifically, patients with more than 10 mm of lateral plateau depression had an eight-fold increase in risk for sustaining a lateral meniscus tear compared to those with less than 10 mm [4]. Similarly, other studies have found that specific thresholds for lateral plateau widening or depression can predict meniscal injuries with high sensitivity and specificity [5-7].
Furthermore, it appears that not only does greater articular depression correlate with higher rates of meniscal injury but also influences functional outcomes. Patients experiencing ≥2mm articular step-off or varus alignment showed worse pain scores despite similar overall functional outcome scores when compared to those without such findings [1].
In terms of predictive value for surgical planning, measurements like lateral tibial plateau depressions exceeding certain millimeters have been suggested as indicators warranting heightened vigilance during operative management due to their association with soft-tissue damage requiring repair [6-8].
Collectively these findings underscore the prognostic significance of accurately assessing articular surface depressions in managing tibial plateau fractures. They suggest a direct relationship between fracture severity—as indicated by depth and width—and both immediate soft tissue complications as well as longer-term degenerative changes within the knee joint.
It should be noted however that while there is strong associative data linking joint depression parameters on imaging to adverse clinical outcomes including OA development and meniscal pathology; causality cannot be fully established through these retrospective analyses alone.
In conclusion, careful evaluation using CT imaging can provide valuable prognostic information regarding potential intra-articular soft tissue injuries accompanying acute tibial plateau fractures. Such insights are crucial for optimizing surgical approaches aimed at restoring mechanical axis alignment and minimizing future risks such as OA development.
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities











Article viewed 805 times
13 Feb 2024
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2024). Schatzker VI tibial plateau fracture with ACL and meniscocapsular injury. Journal of Orthopaedic Surgery and Traumatology. Case Report 14082440 Published Online Feb 13 2024.