Destructive osteochondral fracture of the lateral femoral condyle following traumatic patella dislocation
Score and Comment on this Case
Clinical Details
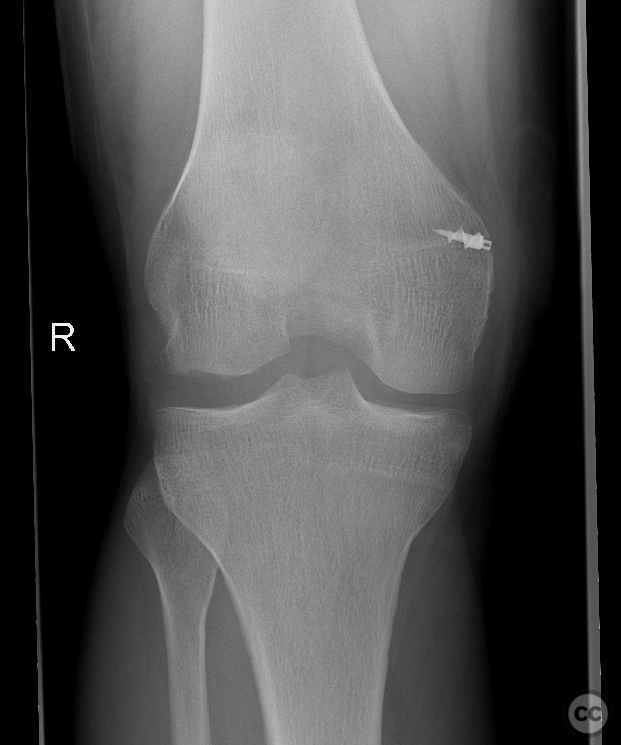
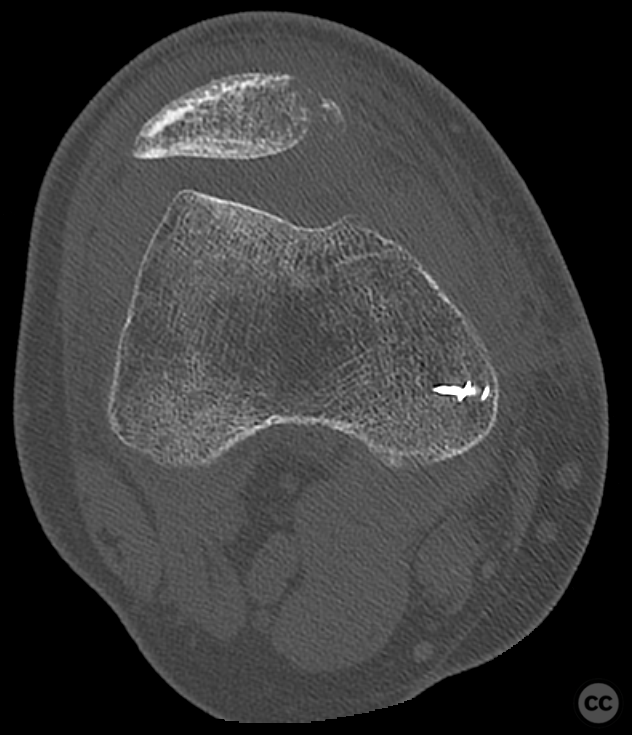
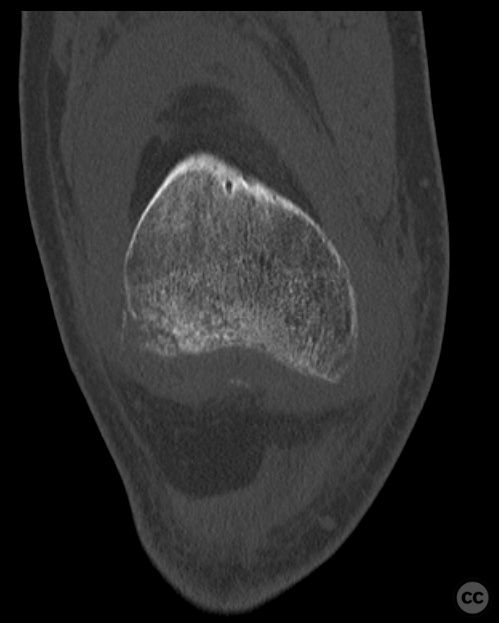
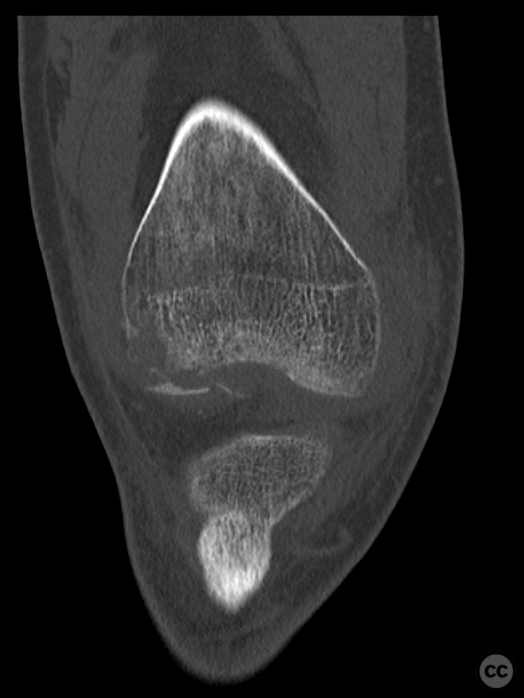
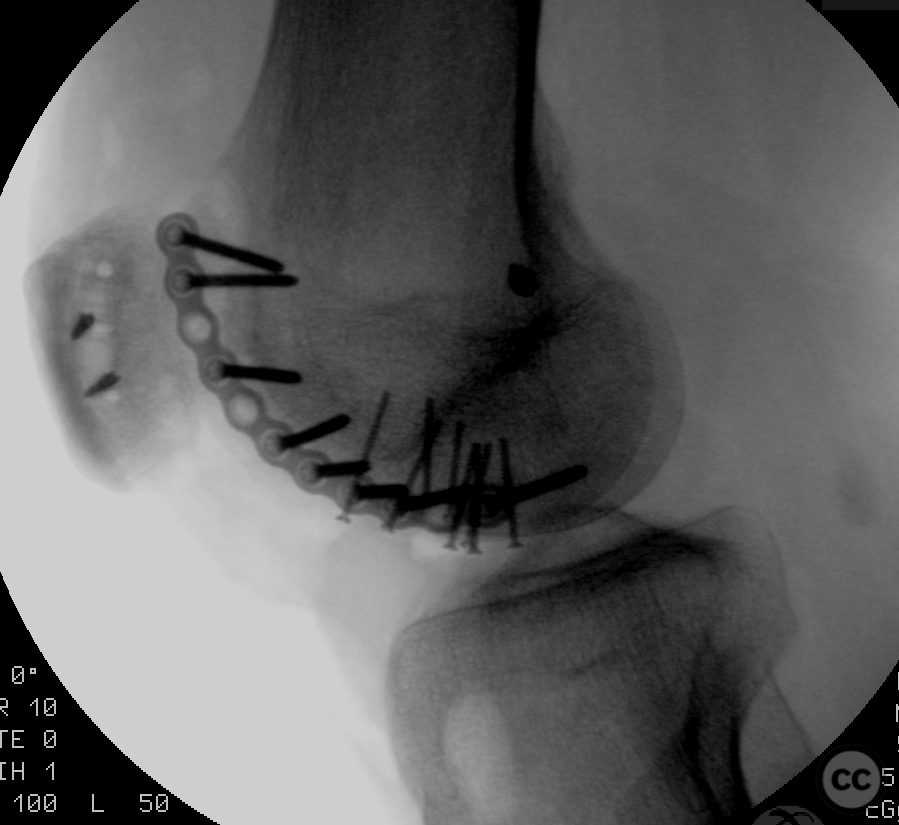
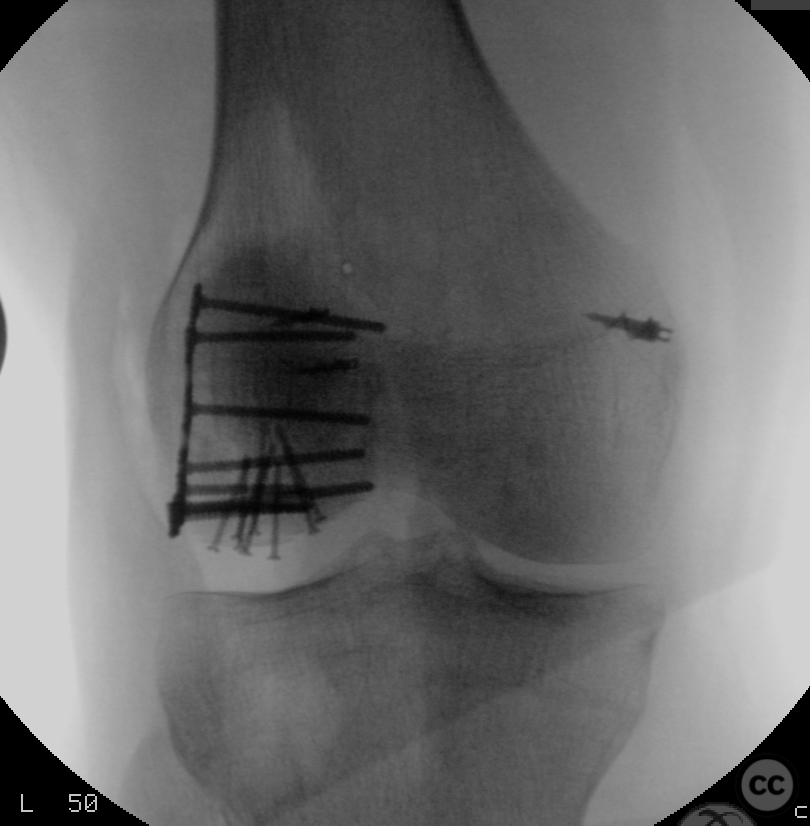
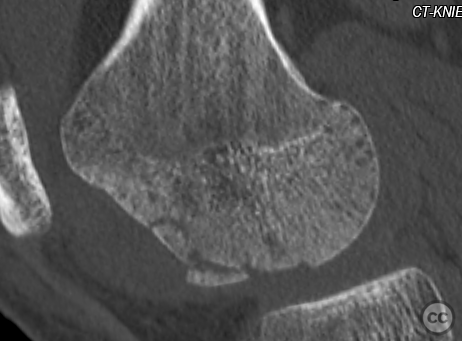
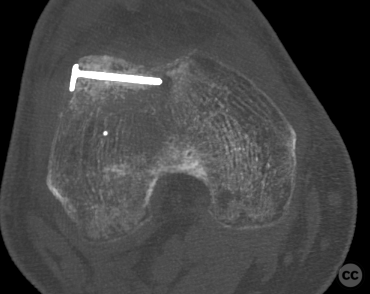
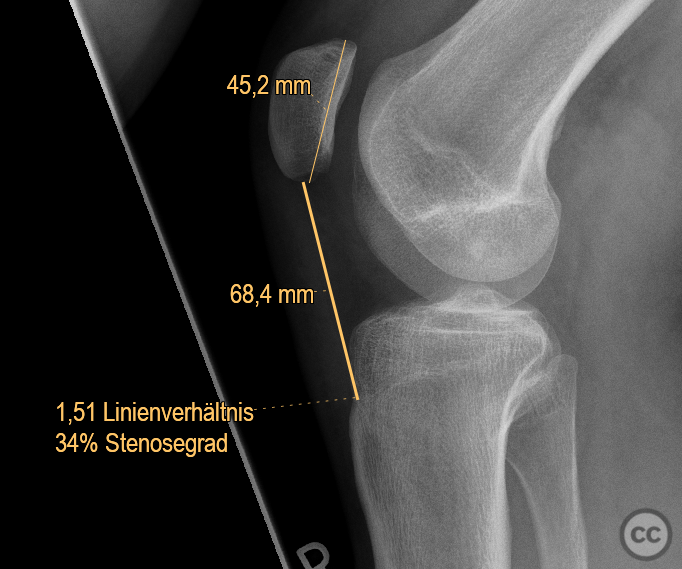
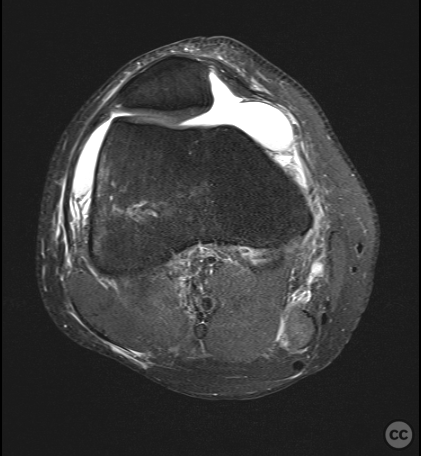
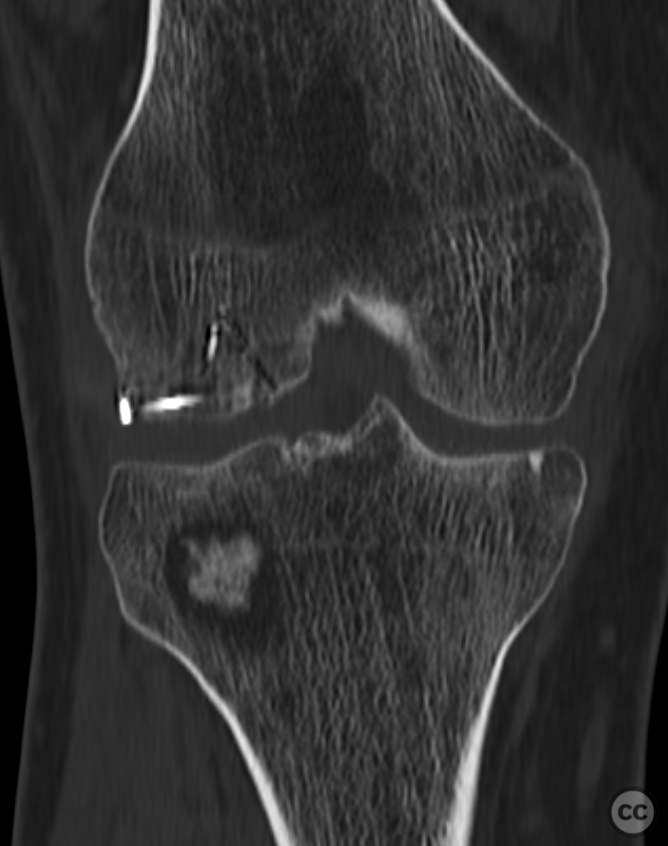
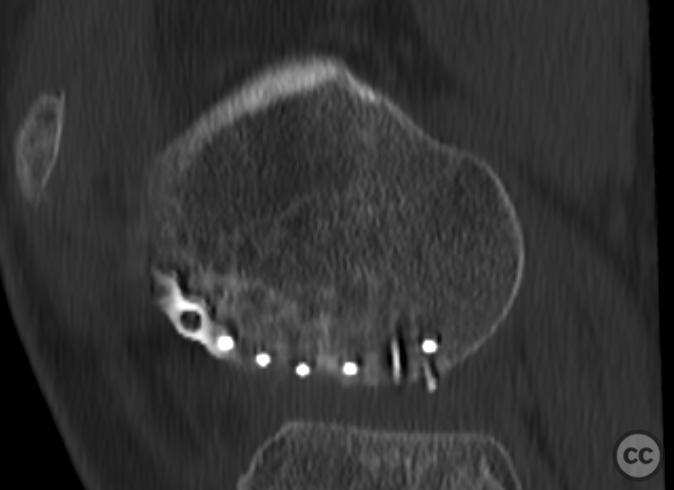
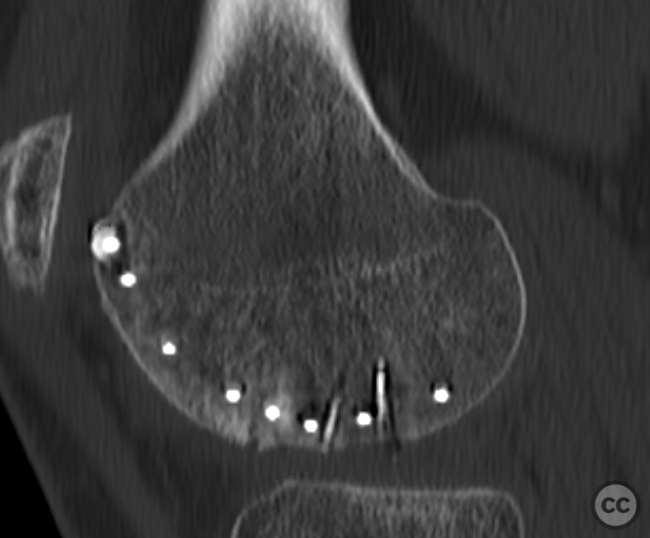
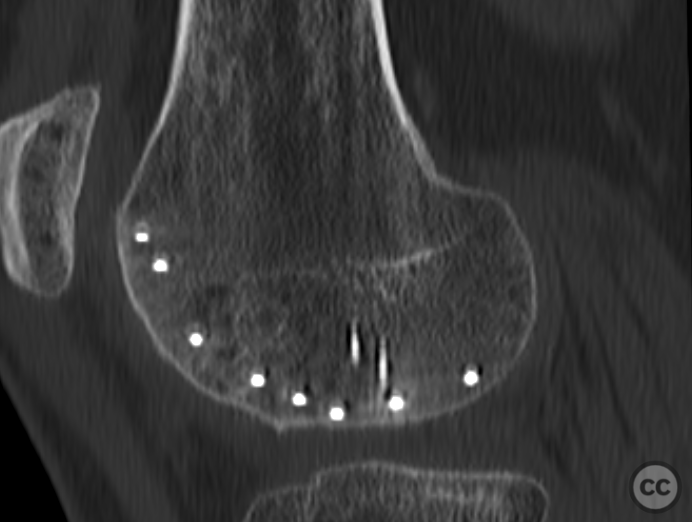
Clinical and radiological findings: This is a mid-20s male who presented following a stumble down several steps. The patient at the time of injury was three months postop femoral MPFL avulsion and subsequent anchor refixation, subsequent to a first episode of traumatic lateral patella dislocation. The initial postoperative course was unremarkable, the patient describing no subjective patella instability or knee problems. The current injury was not sustained because of a recurrence of dislocation rather it appears that in the process of falling, the patella has dislocated laterally with a medial bony avulsion of the medial capsuloligamentous attachment. Additionally evident is a degree of bony injury to the lateral femoral condyle. The extent of this injury was initially underappreciated on imaging, but became evident at time of surgery, which we will see. This patient does have a dysplastic trochlea with medial trochlea hyperplasia, a small thin patella with low lateral patellar facet angle. The Wiberg angle is almost unrecognizable with a soft transition between medial and lateral facets. On the lateral plane films, we can appreciate a marked trochlea bump and although not evident on the presented films, a positive crossing sign .
Preoperative Plan
Planning remarks: Operative management was a planned refixation of the medial bony patellar avulsion along with open refixation of the obvious osteochondral fragment, together with an open assessment of the further bony injury iditifiable on CT. The degree of femoral condylar injury was entirely under appreciated on preoperative CT imaging.
Surgical Discussion
Patient positioning: Supine, with a carbon wedge placed under the heel allowing resting intraop flexion of 90deg
Anatomical surgical approach: Midline incision with lateral parapatellar approach to the lateral femoral condyle.
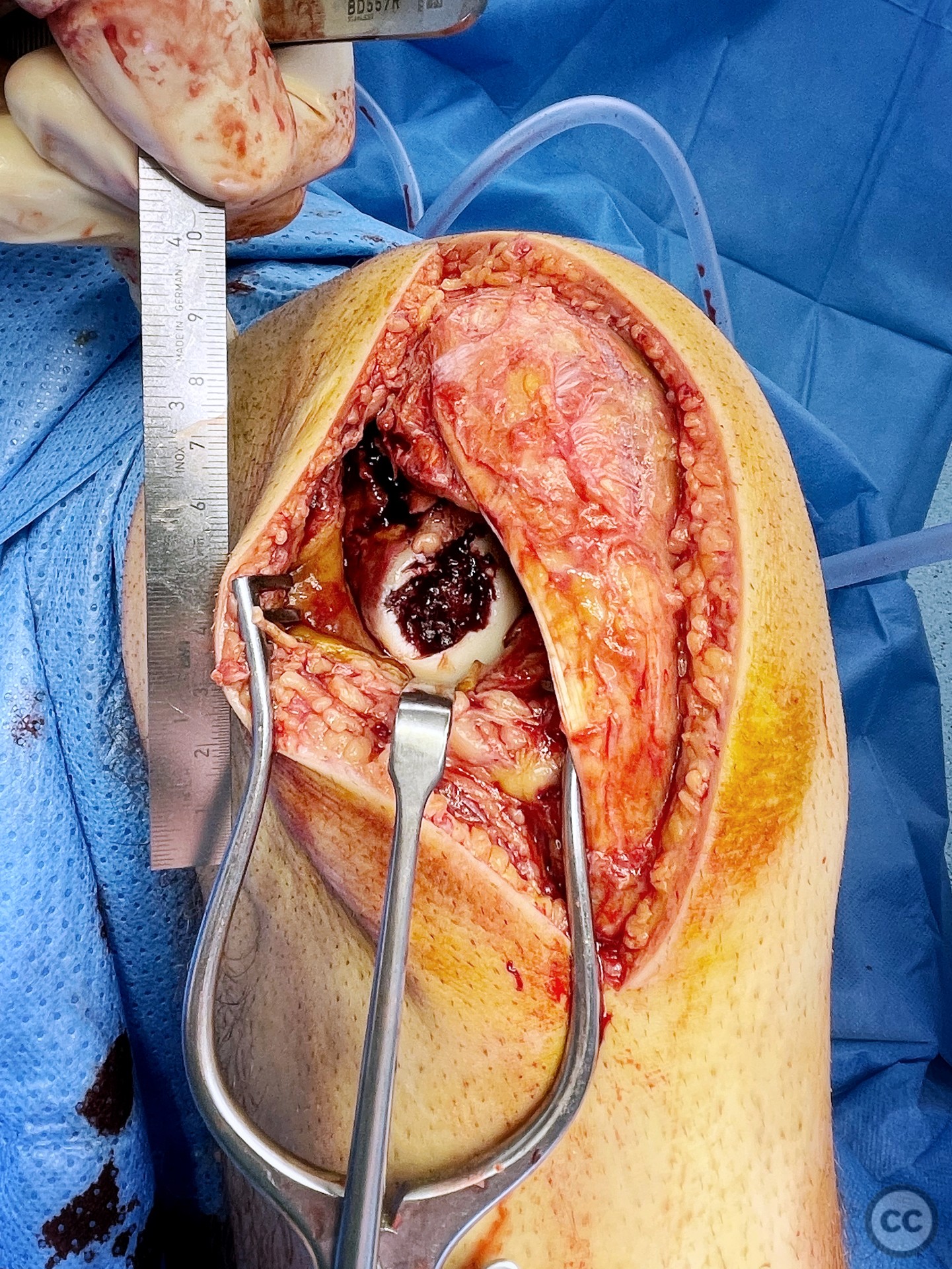
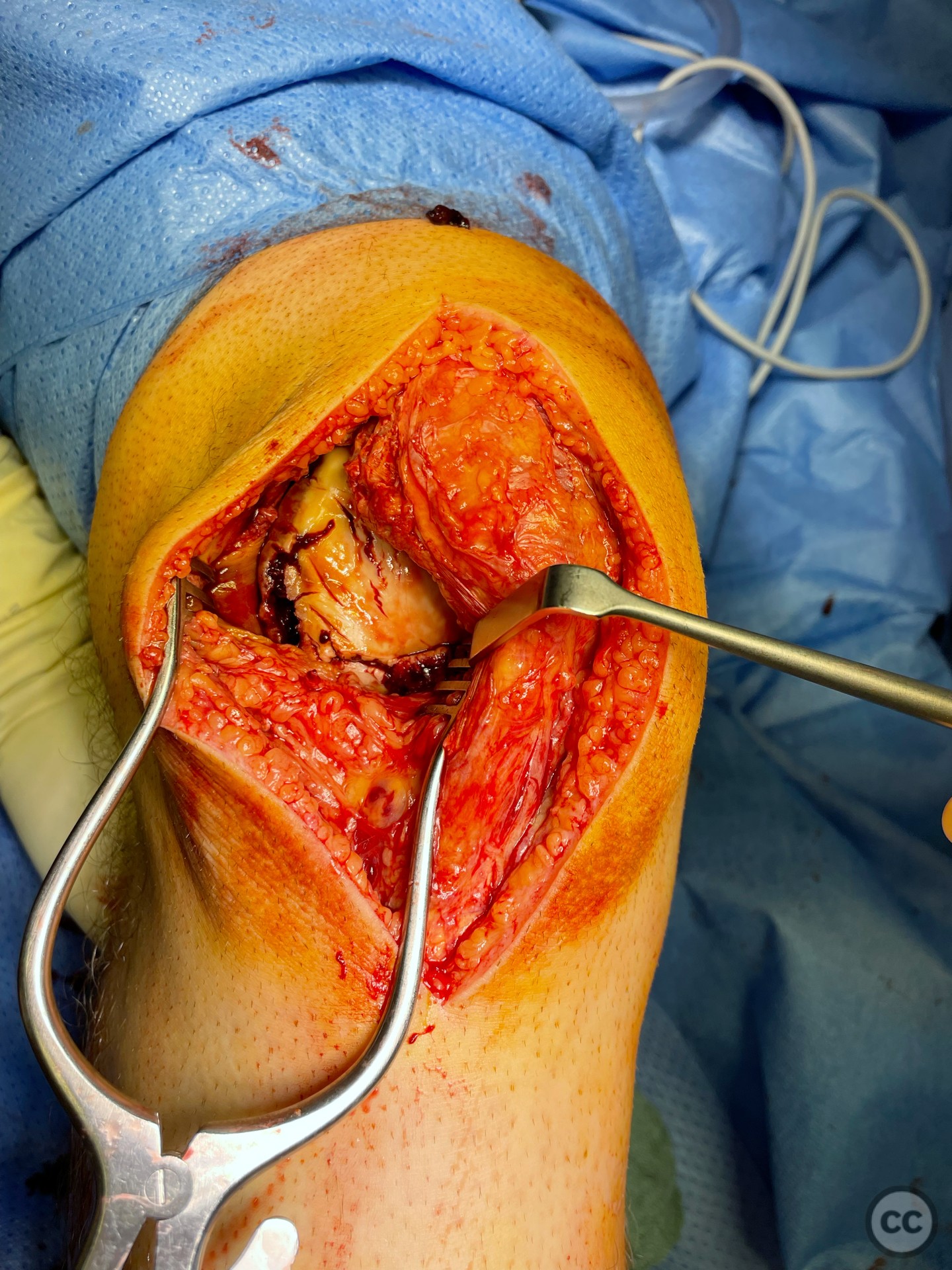
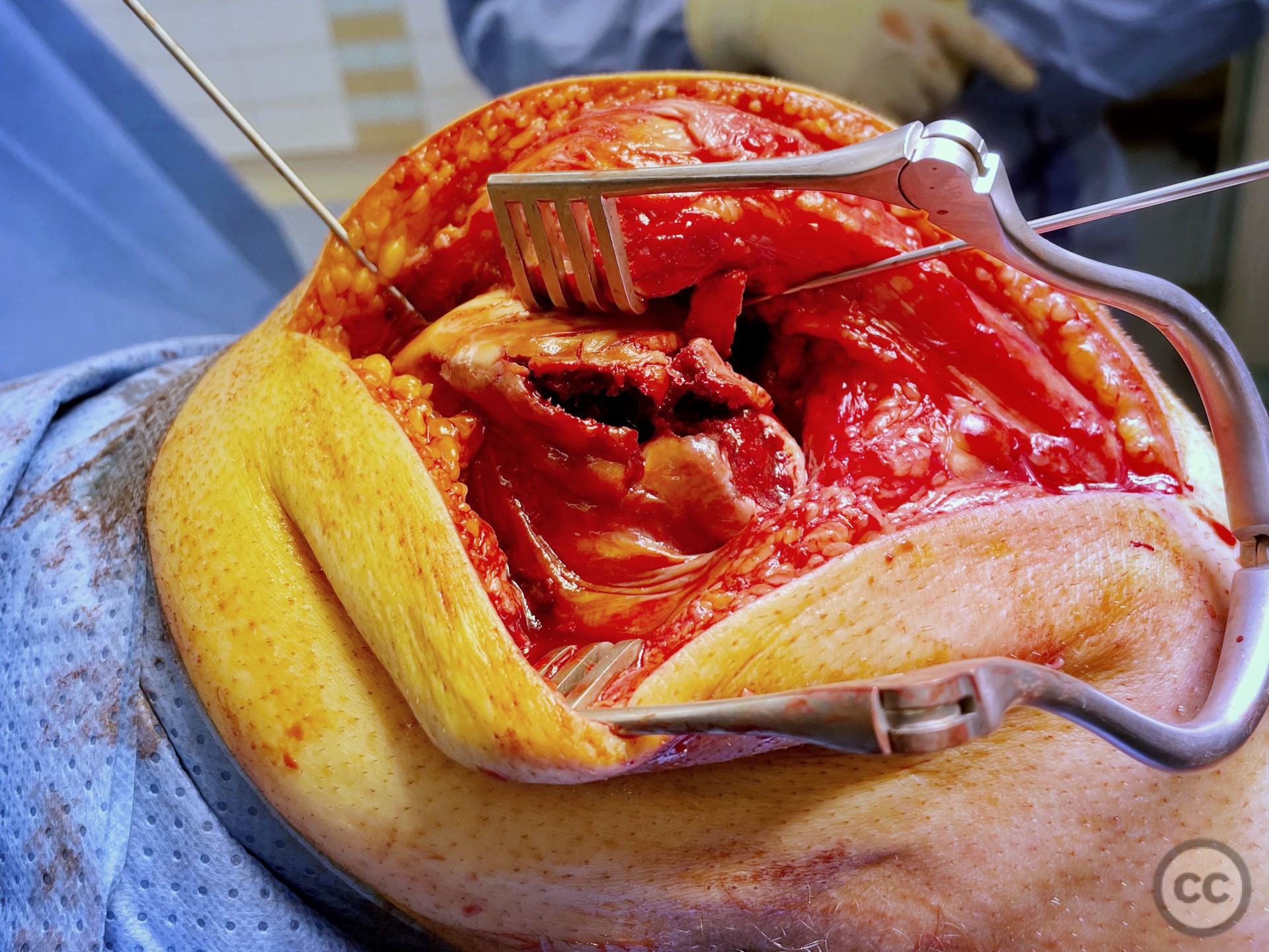
Operative remarks:Operation was done supine on a radio translucent table with a knee flexed to 90° supported by a lateral side support and foot block. A lateral parapatella arthrotomy was made. at first glance, only the distal osteochondral defect zone was visualized in accordance with preoperative planning. However, upon medialisation of the patella, the true extent of destructive impaction of the entire condylar surface became evident.
It’s hypothesized that in a laterally dislocated position the patient has impacted directly onto the patella and the patella then onto the lateral femoral condyle, thereby stamping a 5-10mm deep impression of some 60 x 30 mm. The articular line cartilage in this area was wrinkled and buckled with incomplete tearing. This focal compression of the condyle under the patella caused an extrusion of cartilage and bone distally/posteriorly, causing a sheer injury and creation of the known 15-20mm dia osteochondral fragment from the weight bearing zone of the condyle.
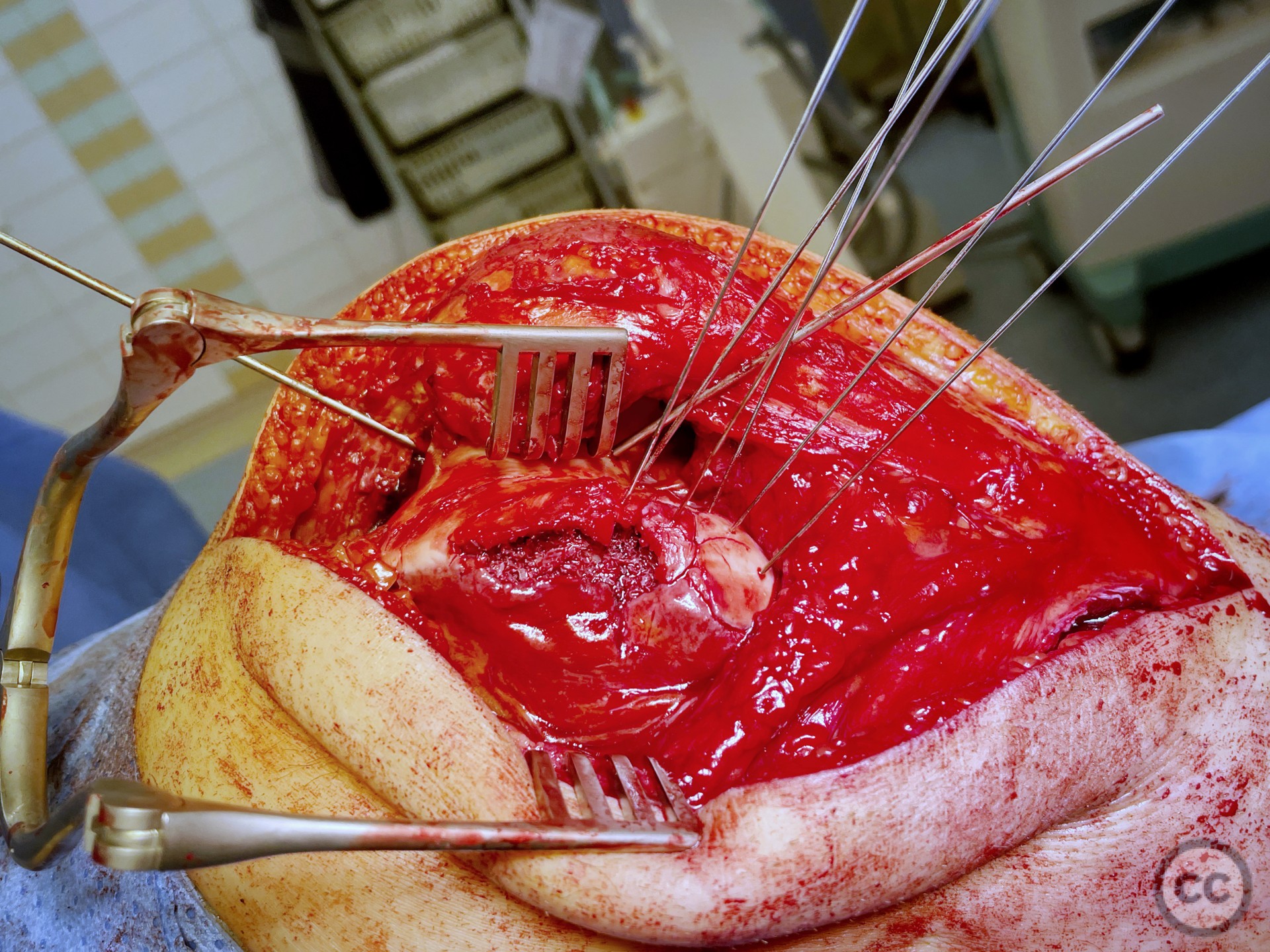
All chondral injury demonstrated significant remaining subchondral bony attachment. We proceeded to create a cortical working window in the lateral condyle through which we disimpacted the 5 to 10 mm of height loss and recreated condylar curvature. Sequential disimpaction of the surface slowly rendered a smooth, congruent, articular surface with large subchondral bony defect.
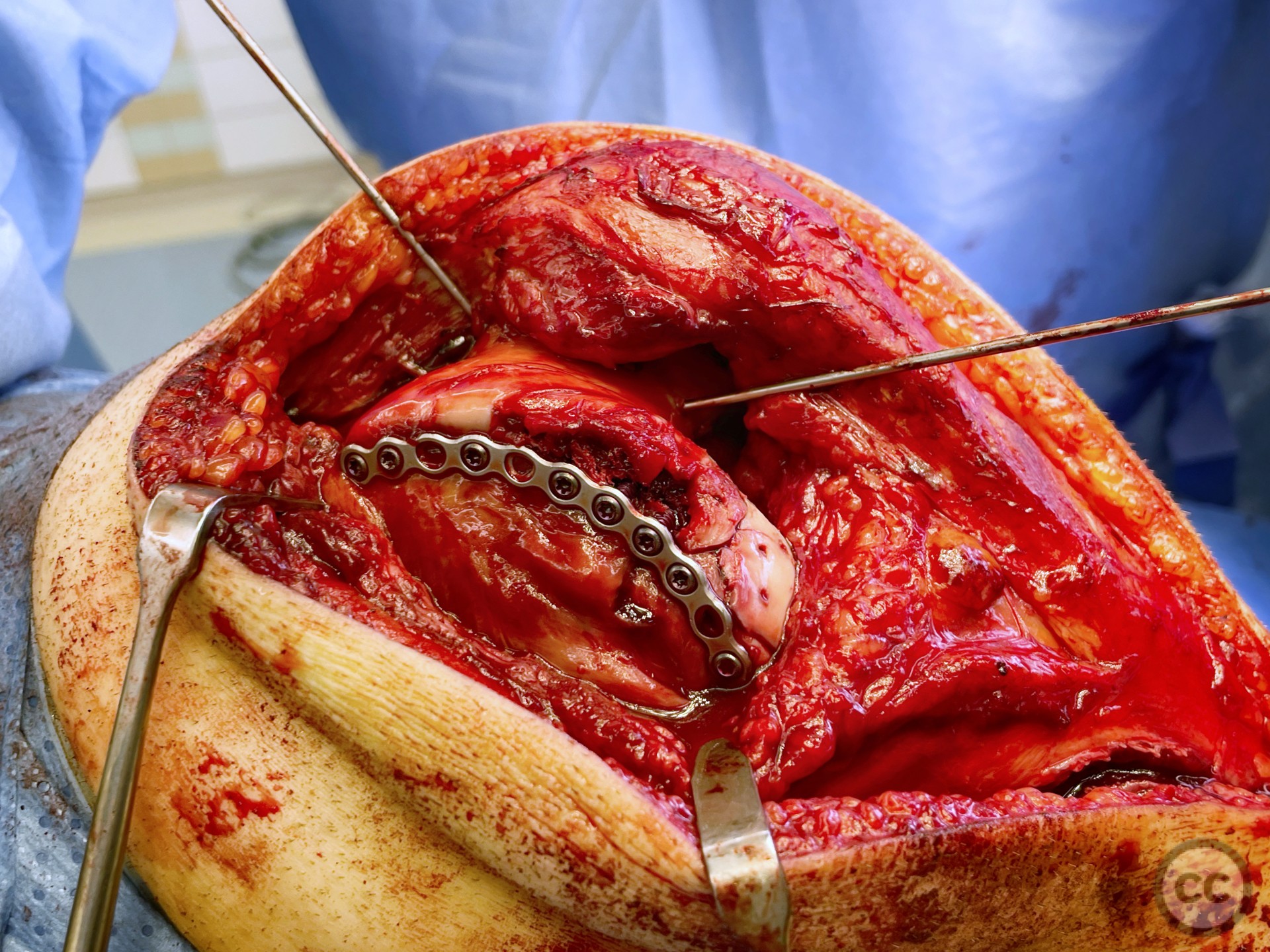
Needing graft we opened a metaphyseal window in the proximal tibia, and harvested a large quantity of cancellous bone. Graft impaction into the defect zone produced a stable, reconstructed articular height. Upon this bony foundation we then sequentially fixed the various chondral fragments using 1.7 mm flat headed Leibinger screws, which were countersunk to 1 to 2 mm below joint surface. Whilst superficially, the contour of the condyle was satisfyingly restored there remained concern over loss of this reduction in the postoperative period. We decided to place a contoured 2.4 mm mini fragment plate to the contour of the lateral articular surface and rafted the subchondral bone with 2.7 mm Locking screws. This provided a stable construct which would be capable of withstanding joint reaction forces during the nonweightbearing recovery period.
The medial bony avulsion of the ligamentocapsular attachments was fixed with two corkscrew anchors. We further medialized the patella through a 10 mm lateral release . The patient will be nonweightbearing for 10 weeks with gradual increase of weight-bearing between 10 to 12 weeks. Range of motion will be initially restricted to 30° for three weeks 60 for the subsequent three weeks with 90° allowed after six weeks.
Postoperative protocol: NWB/TWB for 8 weeks in a ROM Brace, initially locked in 30deg flexion for 2 weeks, followed by 0-30, 0-60 and 0-90 over subsequent weeks. 8 week postop CT slices and clinical AROM attached prior to commencement of PWB. Further follow up will be added in due course.
Orthopaedic implants used: 2.4mm minfragment plate with 2.7mm locking screws. 1.7mm Leibinger screws
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisThe surgical management presented on the webpage involves lateral parapatellar arthrotomy, which exposes the destructive impaction of the entire condylar surface upon medialization of the patella[2]. Osteochondral fractures of the lateral femoral condyle are rare and commonly treated with open reduction[4]. However, removal of free bone fragments has been criticized for causing friction between the defective bone surface and tibia, leading to early osteoarthritis[5].
Alternative approaches for treating osteochondral fractures include fixation with bioabsorbable pins or screws, subchondral bone grafting, and autologous chondrocyte implantation (ACI)[6]. One case study reported successful treatment of a weight-bearing area osteochondral fracture of the lateral femoral condyle (LFC) caused by patellar dislocation using bioabsorbable screws and bone allografting[7],[9]. However, the long-term outcomes of these techniques have yet to be established.
In the case of patellar dislocation, associated injuries such as kissing contusions and shallow trochlear groove may predispose patients to recurrent dislocation[8]. Thus, surgical management should address these risk factors. Trochleoplasty and medial patellofemoral ligament (MPFL) reconstruction may be considered to address patellar instability, while cartilage restoration techniques may be employed for osteochondral defects[6].
In conclusion, while the surgical management discussed on the webpage is a common approach to osteochondral fractures, there is potential for improvement. Treatment of osteochondral fractures with bioabsorbable fixation devices and bone grafting, along with addressing predisposing factors to patellar dislocation, may represent a more comprehensive approach to management. However, further research is needed to establish the long-term outcomes and best practices for these techniques.
Author's Resources & References
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities
















Article viewed 2546 times
09 Dec 2022
Add to Bookmarks
DOI: 10.36438/ORIF2023001 Full Citation
Full Citation
Cite this article:
Oates, E.J. (2022). Destructive osteochondral fracture of the lateral femoral condyle following traumatic patella dislocation. Journal of Orthopaedic Surgery and Traumatology. Case Report 14129311 Published Online Dec 09 2022. DOI: 10.36438/ORIF2023001