Schatzker VI tri-condylar fracture with pseudo PLC disruption
Score and Comment on this Case
Clinical Details
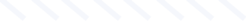
Clinical and radiological findings: This case pertains to a 52-year-old female patient who sustained a right knee injury following a bicycle accident. She was presented to the emergency department with symptoms of pain, evident clinical deformity, and inability to weight bear isolated to the right lower extremity. Radiological examination through plain imaging performed in the emergency department demonstrated a bicondylar tibial plateau fracture with diaphyseal dissociation, consistent with a Schatzker six tibial plateau fracture classification. The significant displacement of the lateral tibial condyle indicated valgus instability. Due to her after-hours presentation, the on-call surgical team decided to mobilize the limb with an external fixator.
Preoperative Plan
Planning remarks: The preoperative plan involved waiting for the consolidation of the soft tissue swelling in the external fixator with definitive management planned on post-injury day 7 to 10. Surgical planning catered to a bicondylar fracture with coronal plane fracture fragments involving the posteromedial and posterolateral condyles. The pattern of injury is consistent with a hyperflexion valgus mechanism. The degree of impaction of the posterolateral corner was highly comminuted. The severe head fracture suggested a possible posterolateral corner menisco-ligamentous injury. The surgical plan was to first stabilize the posterior column, followed by medial column stabilization, and then address the lateral side, with possible exploration of both the anterolateral and posterolateral aspects of the lateral plateau. A ligamentous reconstruction of the posterolateral corner was anticipated.
Surgical Discussion
Patient positioning: The patient was positioned supine, with the leg supported under the distal thigh with a carbon roll, allowing intraoperative flexion of approximately 30 degrees.
Anatomical surgical approach: A two-incision approach with a semi-suspended lower limb allowed approximately 270-degree access around the joint, which made possible a Lobenhoffer approach and direct plating of the posterior column. This minimized the need to reposition the patient from prone to supine intraoperatively, thus saving around 40 minutes of operative time.
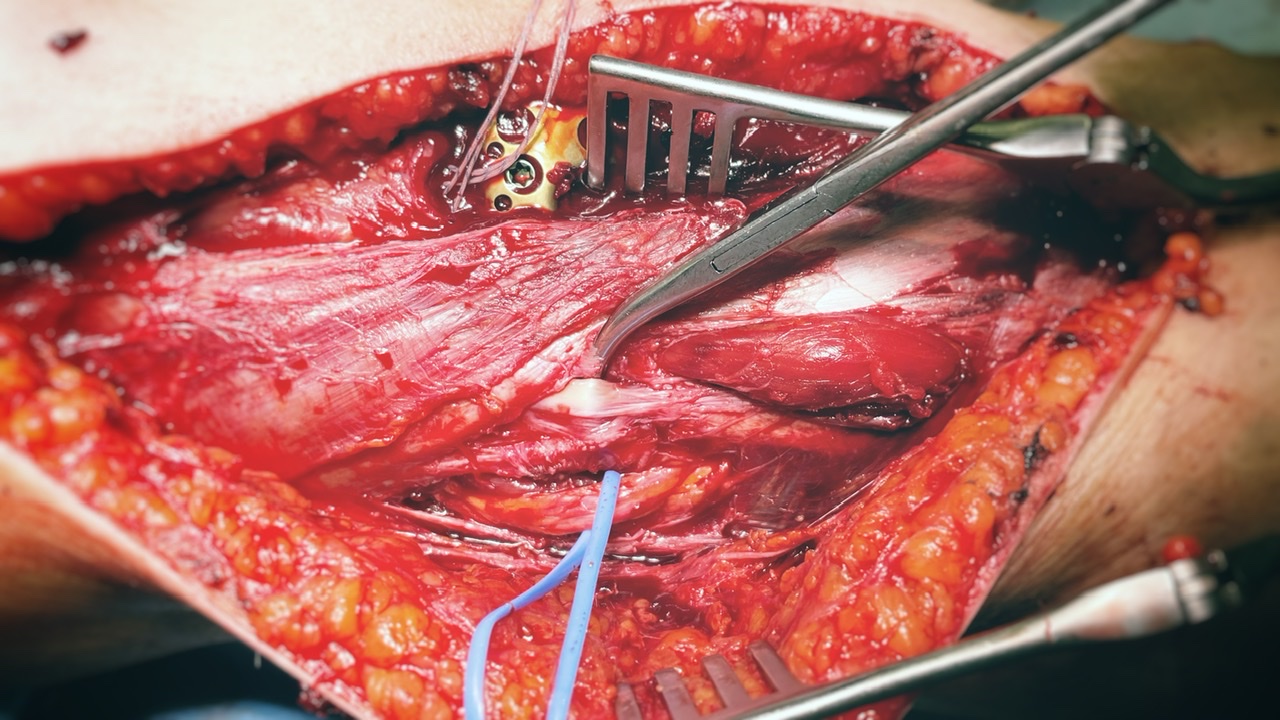
Operative remarks:Following the preoperative plan, the posteromedial approach to the posterior column allowed for the unremarkable plating of the posterior shear coronal fracture with a modified distal tibial locking plate. This distal tibial plate has multiple distal screw options, and the curvature and angulation of the locking screw trajectories fitted this fracture pattern appropriately. After the installation of the posteromedial plate, we shifted to the anteromedial side to provide support for the medial column, using deliberately short anteromedial subchondral screws. This prevented the screw positions from interfering with the reduction and fixation of the lateral condyle.
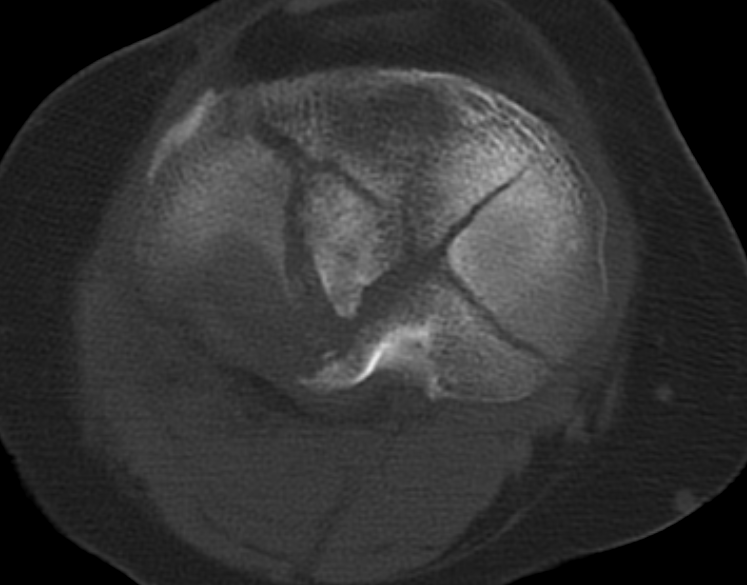
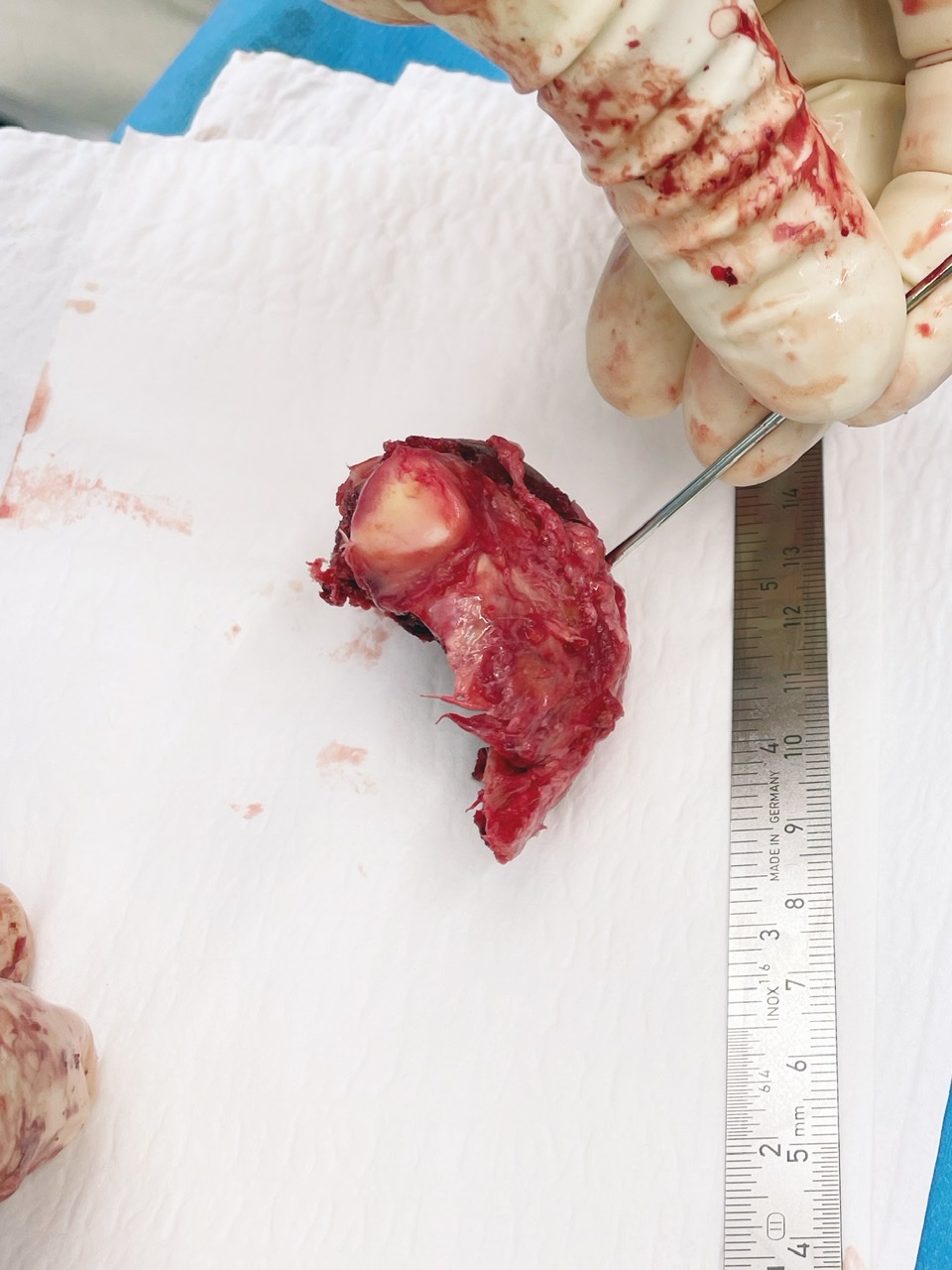
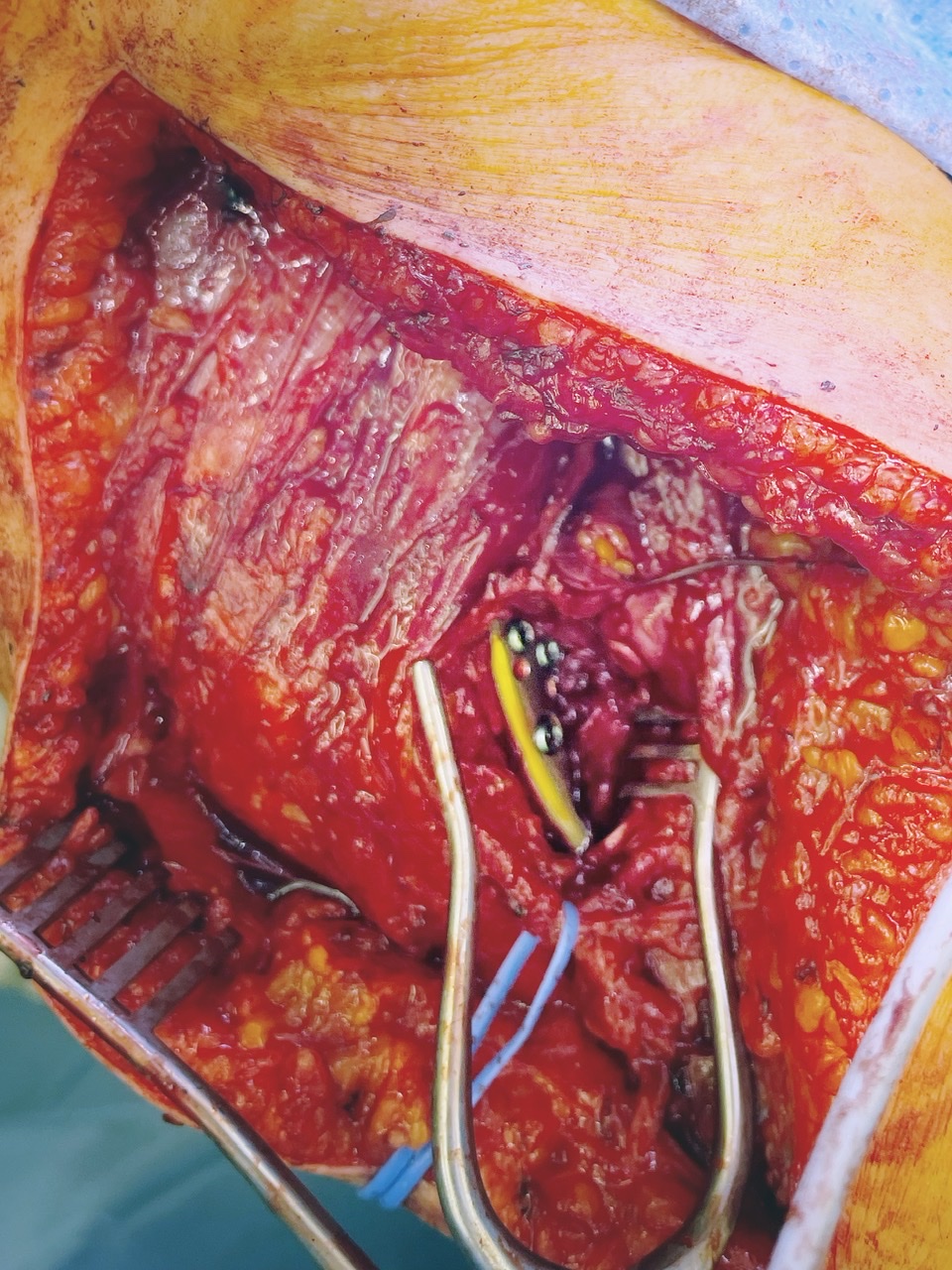
The length of the medial plate was chosen such that the external fixator pins distally were adequately bridged, thus avoiding stress risers and concentration at this previously operated level. The lateral side was intriguing; following soft tissue mobilization and exposure of the lateral condyle fragment, the lateral condyle spontaneously extruded itself from the wound, as visualized in the intraoperative images. This included a visible fibular articular facet as a single free fragment, allowing excellent visualization of the lateral meniscus, which was longitudinally torn. This facilitated direct open suture repair of the meniscus before the reinstallation and fixation of the condyle piece.
Interestingly, following reduction of condyle height and coronal plane alignment of the limb, the crush injury to the fibula head was reduced under indirect ligamentotaxis. While a reconstruction of the posterolateral corner was fully anticipated, the tension of the lateral sided structures following column height reduction was excellent with no residual valgus instability demonstrable intraoperatively. Consequently, no further surgical fixation or reconstruction of the posterolateral corner was required.
Postoperative protocol: The postoperative rehabilitation protocol mandated the patient to remain non-weight-bearing for eight weeks postoperatively. Given the coronal plane stability and lack of injury to the medial and lateral collateral ligaments, no orthotic bracing was necessary. Partial weight-bearing was commenced at eight weeks, gradually increasing to total weight-bearing between 10 and 12 weeks postoperatively. Encouragement of full range of motion started from day one. The postoperative images provided at 12 months postoperatively showed consolidation of the fracture and maintained varus-valgus alignment. Unfortunately, the radiographic projection did not clearly demonstrate the lateral joint surface. However, a minimal loss of height can be appreciated in the lateral projection, while some loss of height in the sagittal plane remains acceptable. The clinical images at 12 months demonstrated no clinically relevant varus-valgus alignment deformity. The patient had a complete pain-free range of motion with full active extension, no extension lag, and active flexion of 130 degrees comparable to the non-operative side.
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® Analysis1. Liangjun et al. conducted a study on non-dislocated hyperextension tibial plateau fractures and reported on the incidence of ligament injuries. They collected data from 25 patients with non-dislocated hyperextension tibial plateau fractures and found that 10 out of 25 patients had ligament injuries. The most common ligament injury was the medial collateral ligament (MCL), followed by the posterolateral corner (PLC) complex and posterior cruciate ligament (PCL) injuries. They also observed that a change in the tibial plateau posterior slope angle of more than 10° was associated with ligament injuries [1]. 2. Herbst et al. discussed ligament injuries in tibial plateau fractures. They emphasized the importance of analyzing the fracture morphology to assess the risk and type of accompanying ligament injuries. They noted that flexion varus fractures are frequently associated with anterior cruciate ligament (ACL) injuries, valgus fractures are prone to medial collateral ligament (MCL) ruptures, and (hyper)extension fractures facilitate posterior cruciate ligament (PCL) and posterolateral corner (PLC) injuries. They recommended using magnetic resonance imaging (MRI) or intraoperative dynamic fluoroscopy to evaluate instability and addressing bony avulsions during osteosynthesis [2]. 3. Yang et al. presented a novel arthroscopically assisted reduction technique for posterolateral tibial plateau fractures. They enrolled 31 patients with posterolateral tibial plateau fractures and reported on the incidence of associated ligament injuries. They found that ACL injuries, including ACL tibial attachment ruptures, occurred in 16 out of 31 patients, meniscus lesions in 19 patients, and MCL injuries in 13 patients. They observed a significantly higher incidence of ACL injuries in the posterior inclination (PI) fracture pattern compared to the lateral inclination (LI) and parallel compression (PC) fracture patterns [3]. 4. Al Sultan et al. presented a case report of a patient with a posterio-latero-central (PLC) sheared fracture of the tibial plateau. The patient underwent surgical repair of the fracture and had a good postoperative recovery without any signs of joint laxity. The case report did not provide specific information about the incidence of ligament injuries in PLC fractures [4]. Based on the analyzed articles, it can be concluded that the incidence of ligament injuries in tibial plateau fractures varies depending on the fracture pattern and associated factors. The incidence of ligament injuries in non-dislocated hyperextension tibial plateau fractures was reported to be 40% [1]. Flexion varus fractures were frequently associated with ACL injuries, valgus fractures with MCL ruptures, and (hyper)extension fractures with PCL and PLC injuries [2]. The PI fracture pattern had a significantly higher incidence of ACL ruptures compared to other fracture patterns [3]. However, there was no specific information on the incidence of ligament injuries in PLC fractures [4].
Author's Resources & References
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant
Industry Sponsership
contact us for advertising opportunities



















Article viewed 1012 times
09 May 2022
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2022). Schatzker VI tri-condylar fracture with pseudo PLC disruption. Journal of Orthopaedic Surgery and Traumatology. Case Report 15436690 Published Online May 09 2022.