Concomitant distal radius and ulna geriatric fragility fracture
Score and Comment on this Case
Clinical Details
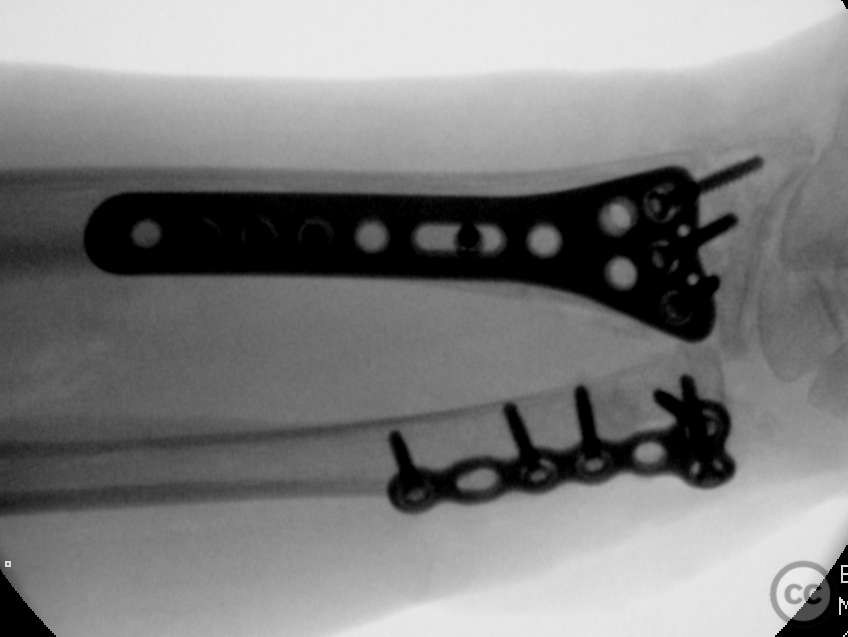
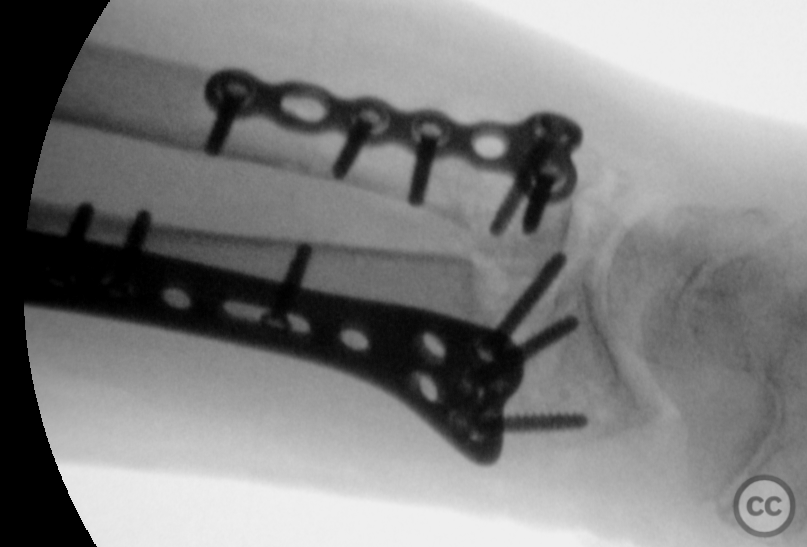
Clinical and radiological findings: This injury belongs to an octogenarian following a simple fall in a nursing home. A closed injury neurovascular status was difficult to determine due to cognitive deterioration. A closed reduction in the emergency department was unsuccessful due to high-grade instability and poor soft tissue envelope. Operation was done on the day of injury. Henry’s approach to the distal radius demonstrated markedly osteopenic metaphyseal bone quality and extraarticular comminution. In addition the width of the distal radial metaphysis was quite small accommodating only a three hole wide plate. Reduction was achieved precariously and held with multiple temporary k-wires pending provisional positioning of the plate. Due to poor bone quality in the diaphyseal-metaphyseal transition zone a long plate was placed into better quality diaphyseal bone proximally. A second working window proximal to the belly of flexor pollicis longus provided exposure for the proximal screw positions. Reduction and fixation of the distal radius did provide initail axial alignment of the distal ulna however this was not dynamically stable. Anterograde intramedullary nailing was not considered to provide adequate fixation. A direct lateral approach to the ulna splitting the interval between ECU and FCU with retraction of the dorsal cutaneous branch of the ulnar nerve provided adequate fracture exposure. This fracture was difficult to control prior to plating. Ultimately transfixation of both the distal and proximal ulna with k-wires into the distal radius were required to provide some temporary stability. Placement and fixation of the 2.4 mm mini fragment plate with 2.7 mm screws provided adequate longitudinal and rotational stability to allow early ROM.
Preoperative Plan
Planning remarks:
Surgical Discussion
Operative remarks:The need for fixation of distal ulna head and neck fractures in combination with distal radius fixation is a point of discussion in the literature. The attached articles provide argument for the conservative management with good functional outcome comparative to operative management. This is not my common practice and only in cases of non-displaced and dynamically stable fracture constellation following radial repair would I consider non-operative management of distal ulna fractures in both bone injuries.
Orthopaedic implants used: Stryker Variax 2.4/2.7mm DRP and 2.4/2.7mm mini fragment plating system
Author's Resources & References
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities



Article viewed 1238 times
10 Nov 2022
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2022). Concomitant distal radius and ulna geriatric fragility fracture. Journal of Orthopaedic Surgery and Traumatology. Case Report 15860846 Published Online Nov 10 2022.