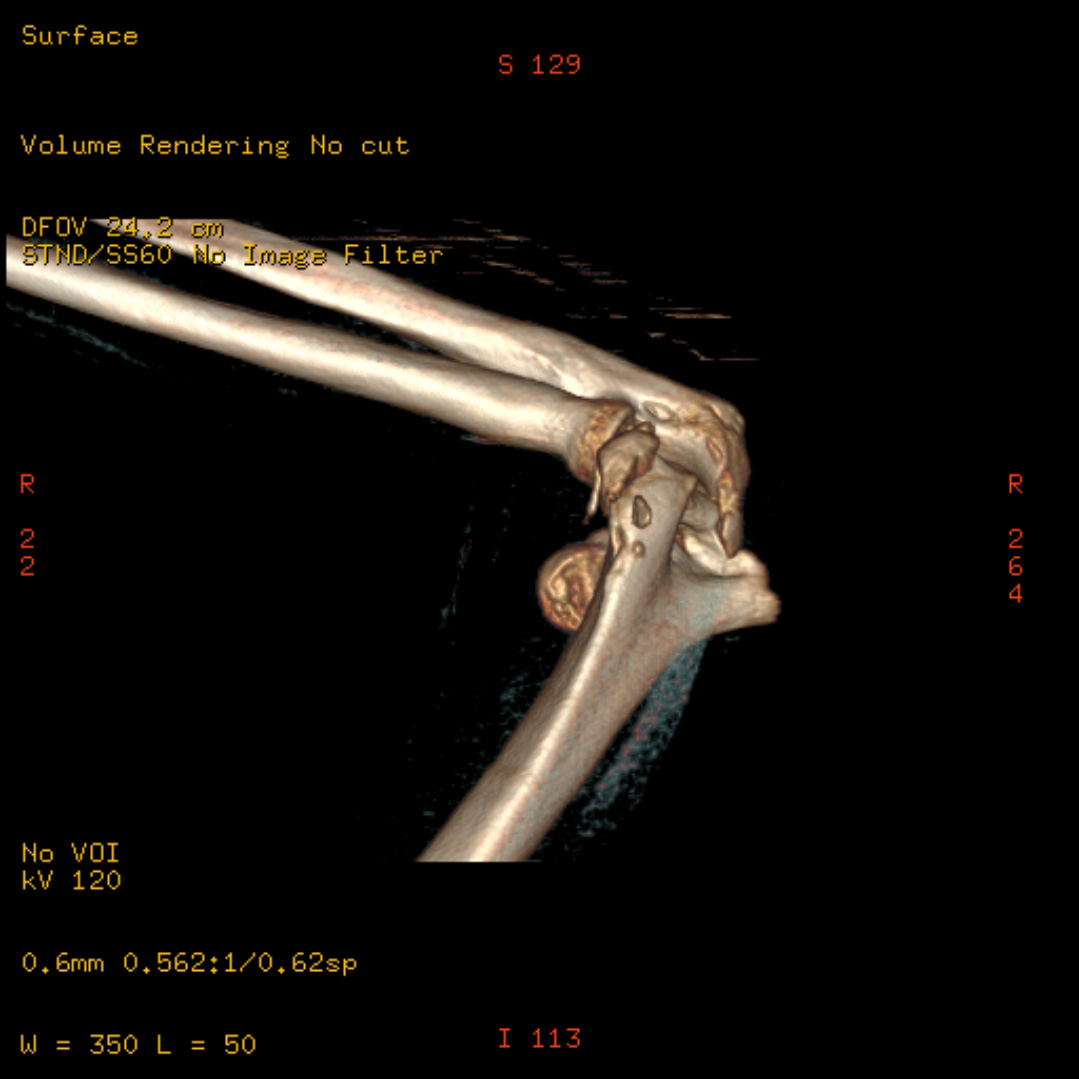
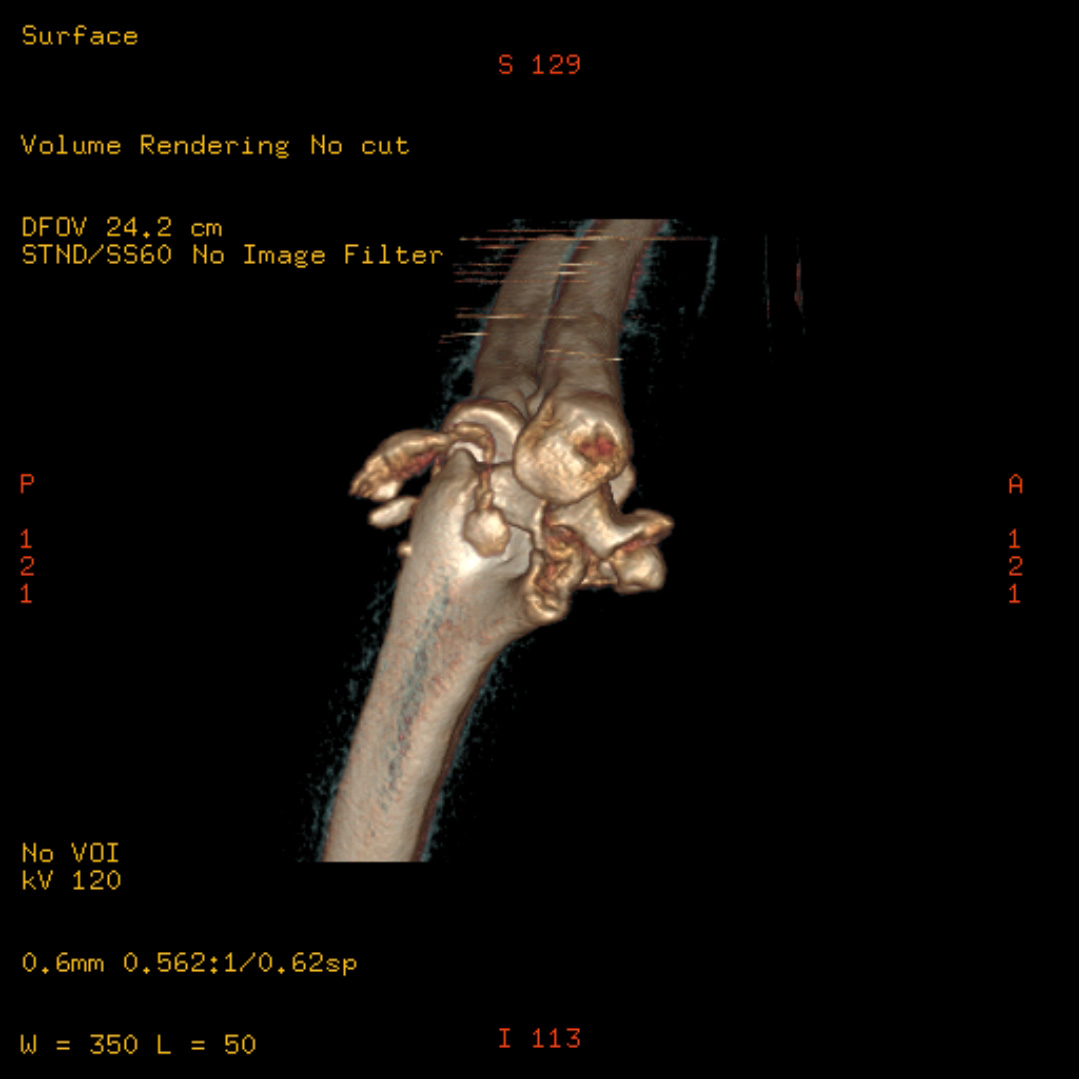
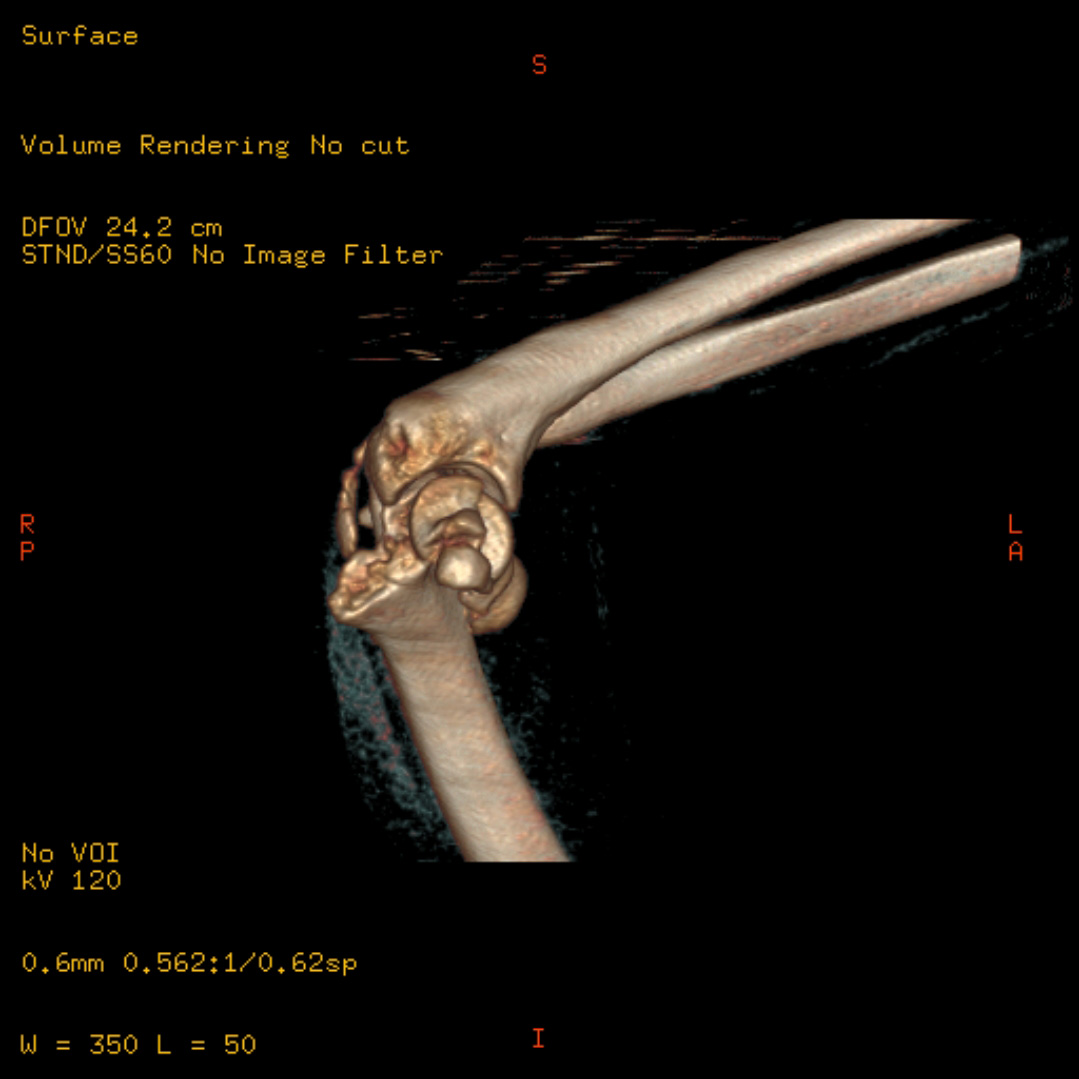
Highly comminuted C3 / Dubberly 3-4B articular distal humerus fracture
Score and Comment on this Case
Clinical Details
Clinical and radiological findings: The case involved a healthy 26-year-old female patient who arrived at the emergency department around 6 PM. A low energy injury, the fracture constellation is absurdly complex - best described as a AO/OTA C3 or more accurately a Dubberly 3-4B. Given the timing of her presentation, a decision was made between immediate surgical intervention or initial immobilisation with postponed definitive fracture management. Ultimately, it was decided to proceed with primary osteosynthesis, with the belief that immediate intervention would yield the best outcome given fresh fracture mobility offering optimal anatomic reduction.
Preoperative Plan
Planning remarks: The preoperative plan was structured around a primary osteosynthesis strategy, aiming to reconstruct the joint fragments into an anatomically coherent structure. The surgery commenced at 8 PM and concluded around midnight, and despite the unorthodox timing, this approach was deemed to be in the patient's best interest.
Surgical Discussion
Patient positioning: Prone with the arm positioned over a small auxiliary arm board, the elbow flexed to 90 deg, hanging towards the floor.
Anatomical surgical approach: Posterior midline incision followed by initial medial and lateral paratricipital windows. During the mobilisation of triceps it became apparent that both the superficial and deep triceps insertion was avulsed from the olecranon.
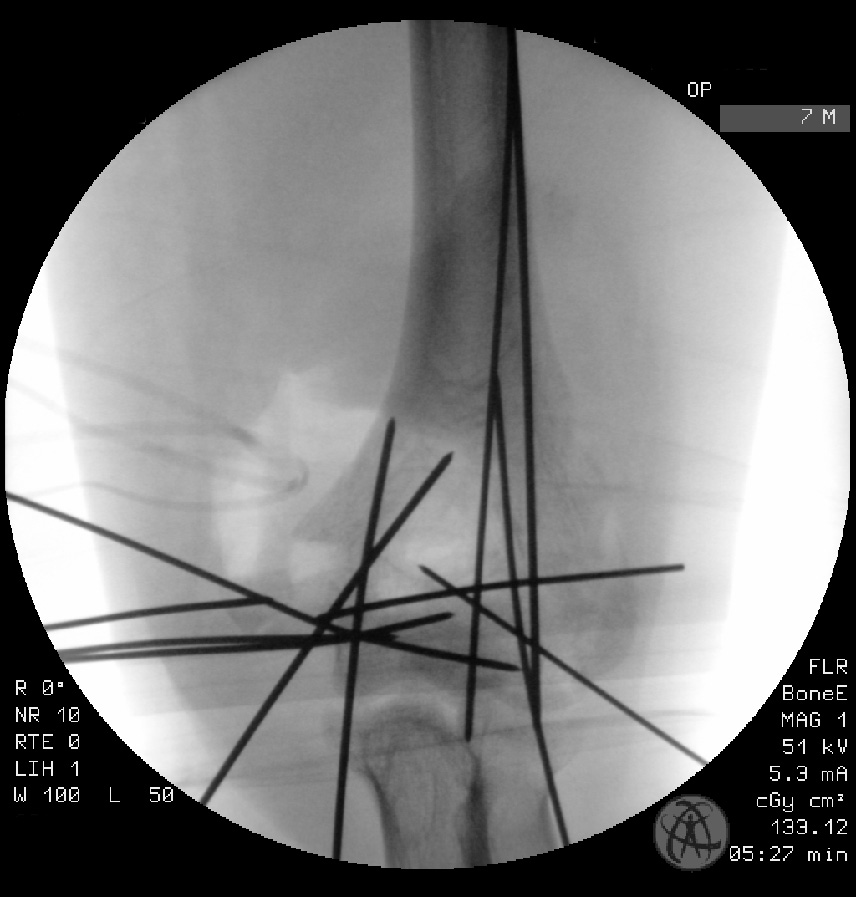
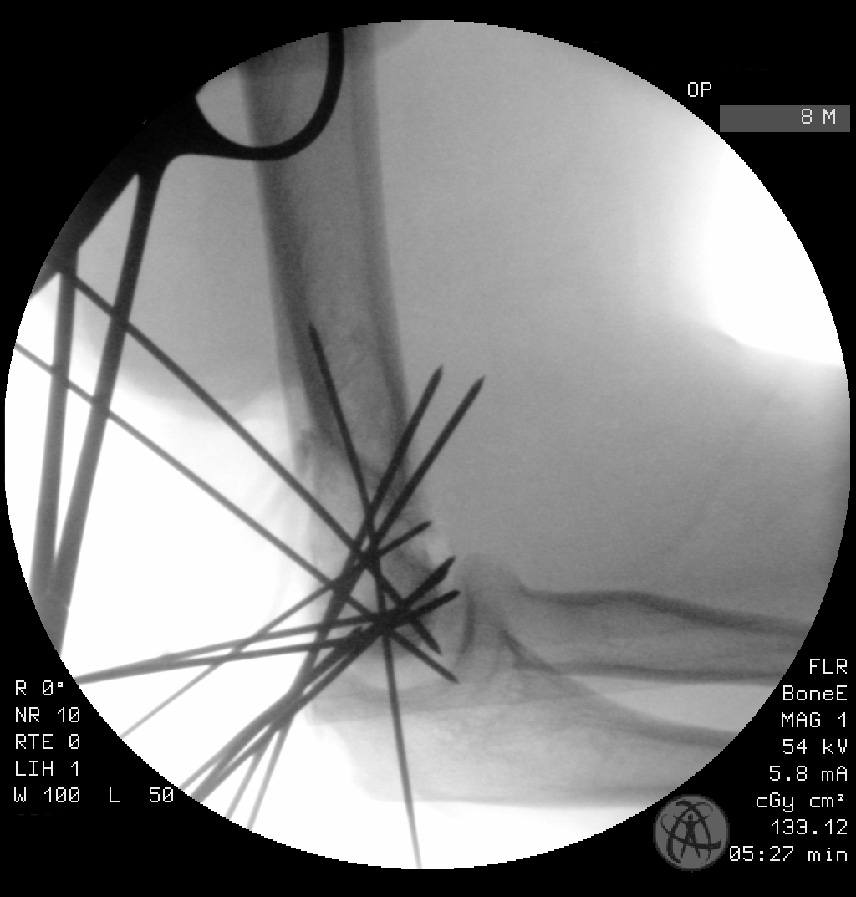
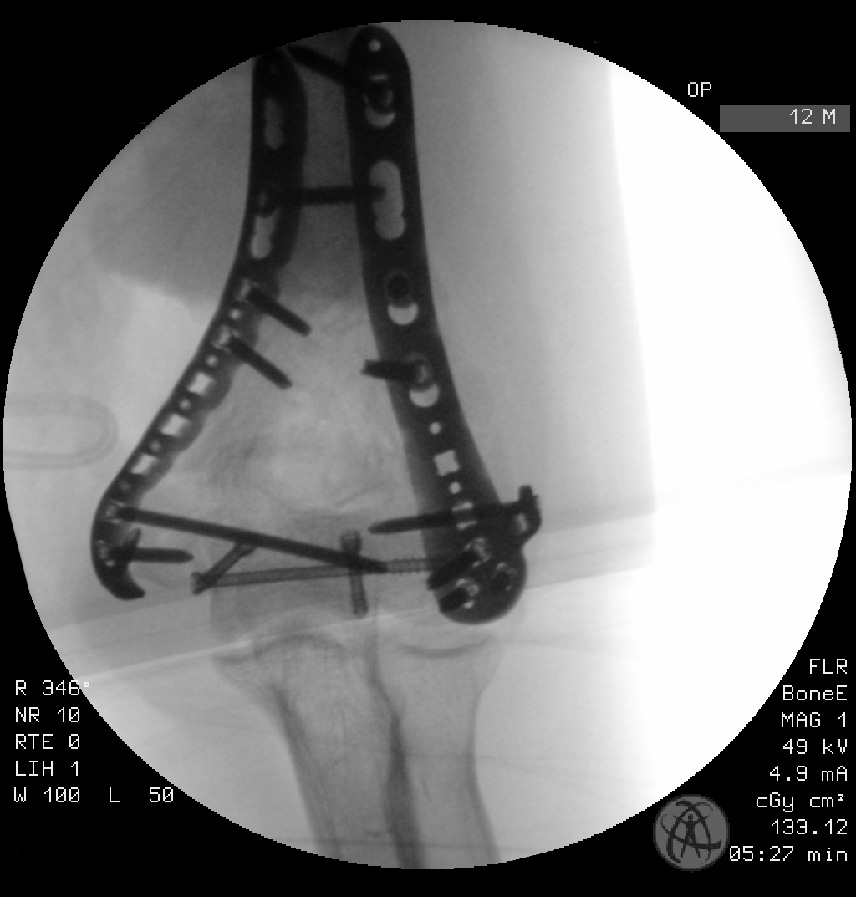
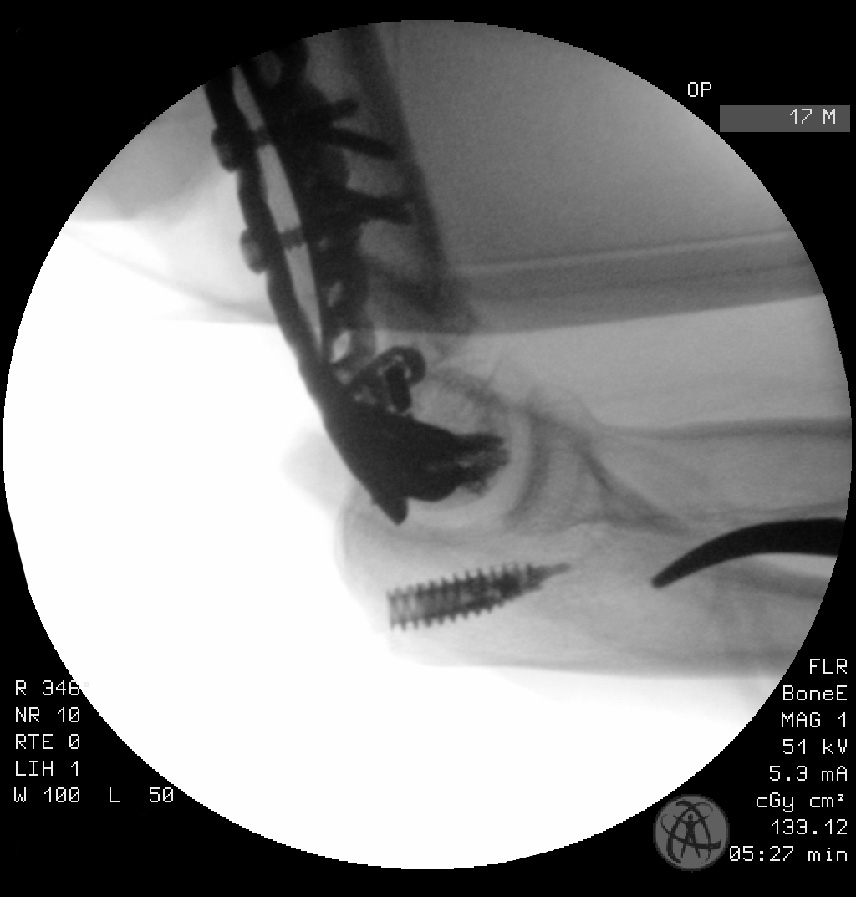
Operative remarks:Post identification and mobilization of the ulnar nerve, and debridement of the joint capsule, approximately 3 to 4 hours were spent reconstructing the joint fragments using 1.2mm Kirshner wires. A radiodorsal plate was placed for capitellum fixation, and the Kirshner wires were sequentially removed. The ulnar component of the coronal shear fracture was fixed using two PA Herbert screws, and a 3mm Asnis cannulated screw was utilized to stabilize the ulnar comminution. Further stabilization of the ulnar column was achieved with an ulnar plate, which adequately maintained the reduction and fixation of the radial and ulnar epicondylar fragments. The triceps were reinserted using two 5.5mm Twinfix/Ultrabraid anchors.
A significant challenge was the inability to restore the condylar-axis to its original ventral position relative to the shaft due to a lack of landmarks and hardware constraints. Despite modifying the plates to improve reduction positioning, the impact was limited. Concerns also existed about the stability provided by the ulna plate to the trochlea, given the complexity of securing meaningful screws via the epicondyle, and the articular surface of the entire trochlea limiting local fixation.
Postoperative protocol: Intraoperatively, a stable range of motion (ROM) of 10-130 degrees was achieved. Postoperatively, an EpicoROM brace was utilized to protect the ROM, with a gradual increase in active range of motion over a 6-8 week period.
Orthopaedic implants used: The orthopaedic implants used in this surgery included 1.2mm Kirshner wires, a radiodorsal plate for capitellum fixation, two PA Herbert screws, a 3mm Asnis cannulated screw for ulnar comminution stabilization, an ulnar plate for ulnar column stabilization, two 5.5mm Twinfix/Ultrabraid anchors for triceps reinsertion, DePuy Synthes VA-LCP Distal Humerus Plates 2.7/3.5mm, and HBS Midi headless screws from KLS Martin.
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisThe studies included in the analysis provide evidence supporting the use of plate fixation in terms of clinical outcomes, functional outcomes, and stability. The first study compared the clinical outcomes of two methods of olecranon repair following distal humerus fracture repair. The study found that patients undergoing tension band wiring (TBW) or plate fixation (PF) for repair of an olecranon osteotomy had similar outcomes in terms of osteotomy time to union, elbow motion, Mayo Elbow Performance Index (MEPI) scores, and complication rates [Haglin et al., 2021]. This suggests that both TBW and PF can be considered when selecting a construct for olecranon osteotomy repair. The second study evaluated the functional outcome of distal humerus fractures treated with open reduction and internal fixation using bicolumnar plating. The study found that excellent to good functional outcomes were achieved in around 80% of the study group, indicating the effectiveness of bicolumnar plating in achieving stability and a good range of motion [Jagadish et al., 2023]. The third study investigated the feasibility of minimally invasive plate osteosynthesis (MIPO) for distal humerus fractures. The study concluded that the MIPO technique for reduction and plate fixation in distal humerus fractures is feasible [Hofmann et al., 2023]. Although this study cannot be clearly classified into a specific level of evidence, it provides valuable insights into the feasibility of MIPO. The fourth study aimed to evaluate the risk factors for stiffness after distal humerus plating. The study identified older age, AO type C2-3 fracture, and injury-surgery interval longer than 7 days as significant risk factors for stiffness [Tunalı et al., 2018]. This highlights the importance of considering these risk factors when planning surgical treatment for distal humerus fractures. In summary, the available evidence suggests that plate fixation, including tension band wiring and plate fixation with olecranon osteotomy or bicolumnar plating, can lead to favorable clinical and functional outcomes in the treatment of distal humerus fractures. However, it is crucial to consider individual patient factors, such as age and fracture type, when selecting the appropriate treatment approach.
Author's Resources & References
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities















Article viewed 1286 times
19 Mar 2021
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2021). Highly comminuted C3 / Dubberly 3-4B articular distal humerus fracture. Journal of Orthopaedic Surgery and Traumatology. Case Report 16720072 Published Online Mar 19 2021.