A tale of 2 pins
Score and Comment on this Case
Clinical Details
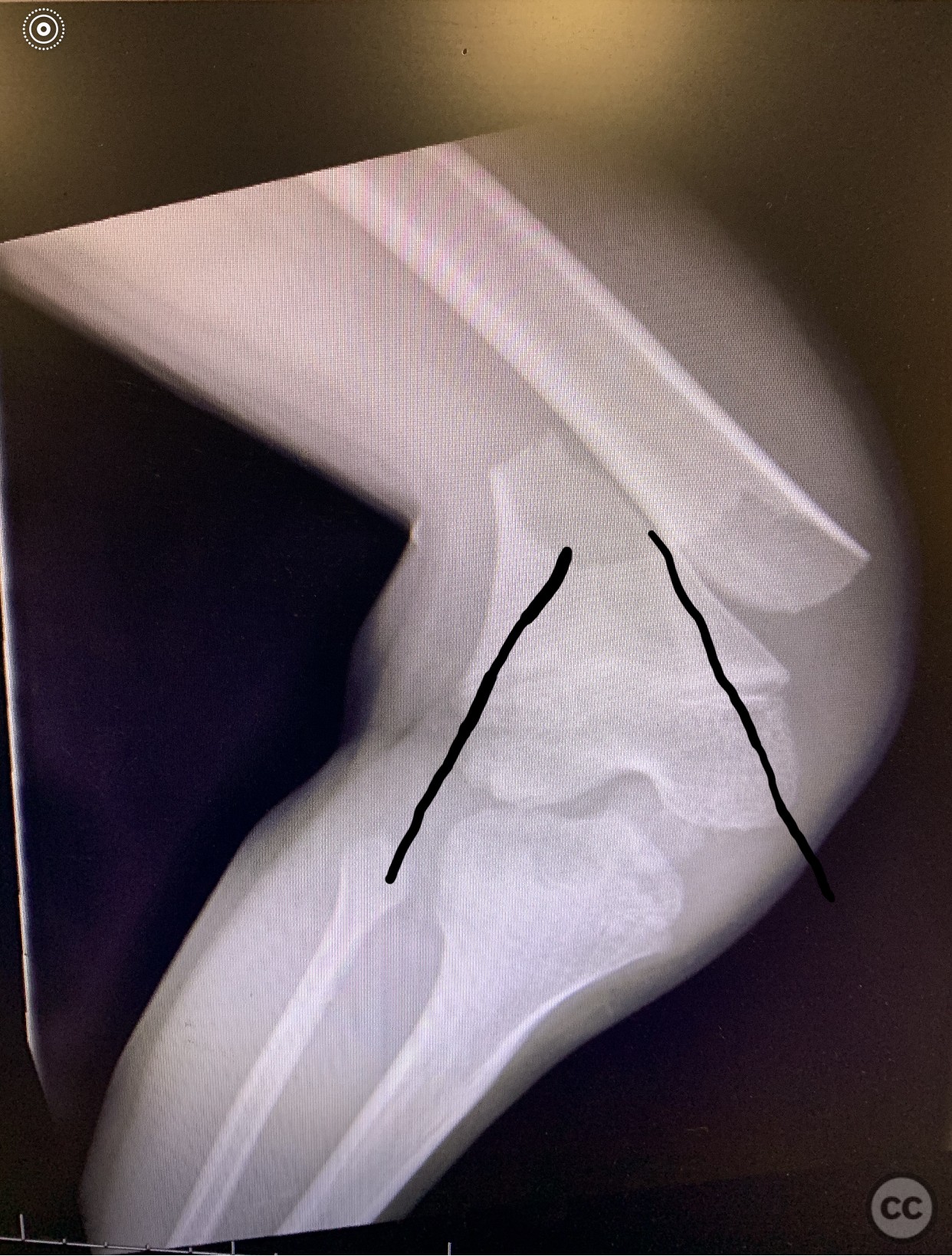
Clinical and radiological findings: 9yo w/ extraphyseal distal femur short oblique fx. Clinical and radiological findings: The radiographic image of the pediatric patient presents an extra-articular distal femur fracture that is noticeably situated above the growth plate, thus being identified as open physis. There is a clear short oblique line of fracture that extends proximally from the growth plate, showing a distinct separation without any signs of fragmentation or comminution. The fracture appears confined within the bone envelope, implying a closed nature of the injury. The integrity of the growth plate appears maintained with no fracture involvement, thereby potentially reducing any interference with future growth. The absence of further abnormalities and the preserved alignment of the bone imply an optimistic prognosis for effective healing with suitable management.
Preoperative Plan
Planning remarks: Preoperative Plan: **Instruments and Implants needed:** 1. 2.5 mm Steinmann Pin: This will be used as a retrograde intramedullary pin for fracture fixation. 2. Orthopedic drill: Required for making the entry point for the pin. 3. Pin introducer: To help guide the Steinmann pin into the femur. 4. Image intensifier (C-arm): For intraoperative radiographic control. 5. General orthopedic instrument set: Including scalpel, forceps, osteotomes, rongeurs, retractors etc. **Operating Room Preparation:** 1. The operating room should be adequately sterilized, well-lit, and equipped with all necessary devices like the operating table, anesthesia machine, and monitoring devices. 2. The C-arm should be positioned on the side opposite the surgeon for easy maneuverability. 3. A radiolucent operating table would be ideal to facilitate intraoperative imaging. **Patient Set-Up:** 1. The patient is positioned supine on the operating table. 2. The involved limb should be free to allow for manipulation and C-arm usage. 3. The limb should be prepared and draped in a sterile manner. **Considerations before Surgery:** 1. The general health status of the patient should be considered, with any comorbidities optimally controlled. 2. Previous imaging studies should be reviewed for a better understanding of the fracture and planning the fixation. 3. A full physical examination should be done, paying particular attention to the neurovascular status of the involved limb. 4. The risks of delayed union, non-union, and potential growth disturbances should be considered **Discussion for Consent:** The surgeon should explain to the patient and their guardians: 1. The nature of the fracture, its location, and its implications. 2. The need for surgery and the process of retrograde Steinmann pin fixation. 3. Potential risks and complications, such as infection, nonunion, malunion, or possible effects on growth. 4. The expected postoperative course including rehabilitation and follow-up appointments. The patient and their guardians should have all questions answered and feel comfortable with the planned procedure before proceeding.
Surgical Discussion
Patient positioning: Supine on a skytron vascular Radiolucent diving board
Anatomical surgical approach: Close restrograde from lateral aspect of intra articular surface to proximal to Fx site with maximal pin spread.
Operative remarks:**Step 1: Anesthesia and Positioning:** The patient is given general anesthesia or regional anesthesia based on the anesthesiologist's discretion.
Once asleep, the patient is positioned supine on the radiolucent table to facilitate C arm usage. The affected leg is prepared and draped in a standard sterile manner.
**Step 2: Identifying Landmarks:** The fracture site is palpated and confirmed using fluoroscopic guidance, with attention to the patella, distal femoral epiphysis, and the site of the distal femoral metaphysis just above the growth plate. The entry point for the pin is typically chosen on the anterolateral aspect of the distal femur. **Step 3:
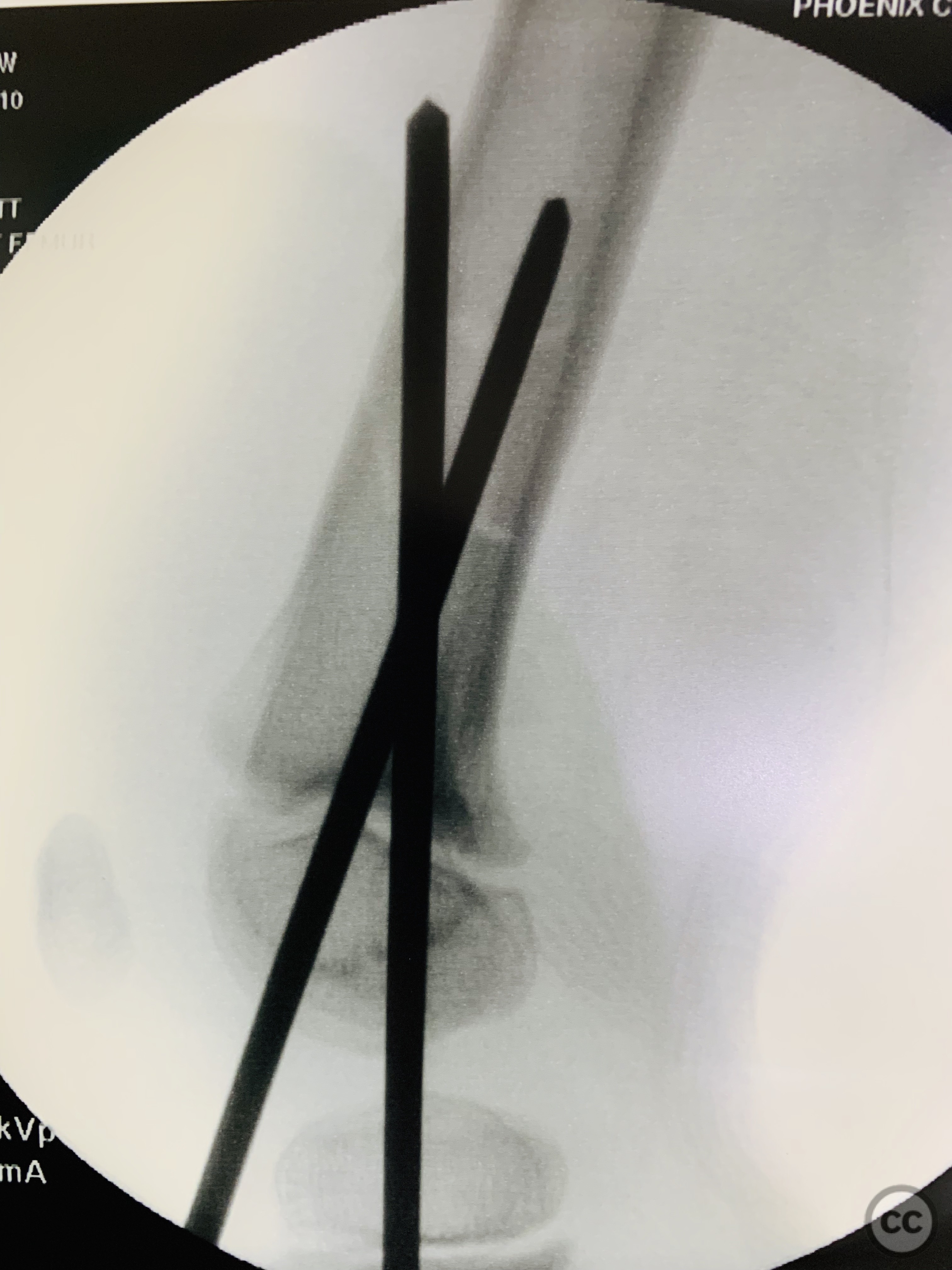
Making the Entry Point:** A small skin incision is made at the entry point. The periosteum is pierced with a sharp awl or drill. The entry point should be cortical, not physeal, to avoid damaging the growth plate. **Step 4: Introduction of the Steinmann Pin:** The Steinmann pin is introduced into the femur in a retrograde manner, from distal to proximal, across the fracture site. The pin is carefully advanced under C-arm guidance to confirm that it traverses the fracture, doesn't cross the fracture site and has maximal pin spread in both planes at the fracture site. **Step 5: Reduction and Pin Placement:** The fracture is then reduced under direct imaging and the pin is further advanced across the fracture site and into the proximal femur fragment.
Often, two pins are used, placed in a cross-pin configuration for better stability. It is okay to enter the joint on lateral side and medial side. **Step 6: Confirming Placement:** Once satisfactory placement is confirmed under imaging, the pin is cut and the skin is closed with absorbable sutures. **Step 7: Post-operative Care:** The leg is often immobilized in a long leg cast or brace for added stability. Post-operative X-rays are taken to confirm good position of the pins and satisfactory alignment of the fracture. **Anatomical Considerations:** Special care is taken to avoid the physis or growth plate, as damage can lead to growth disturbances. The pin should also not breach the joint, as this could cause joint damage or provoke an intra-articular infection. The neurovascular bundle, located medially, should be avoided while inserting the pin from the anterolateral aspect. **Special Considerations:** In pediatric patients, bone healing is generally faster, but proper reduction and stable fixation are crucial to avoid growth disturbances. Rehabilitation and follow-up appointments are critical to monitor healing and check for complications.
Postoperative protocol: **Pin Pull Protocol:** The pin pull protocol typically involves removing the Steinmann pins in a clinic setting once adequate healing of the fracture is confirmed. This typically occurs several weeks to a few months postoperatively, based on radiographic evidence of fracture healing and clinical evaluation of pain and function. The protocol might involve: 1. **Preparation:** The area around the pin site is cleaned with a suitable antiseptic. 2. **Removal:** Using sterile technique and a pin puller or a similar instrument, the pins are carefully removed. Local anesthesia may be used if necessary. 3. **Post-removal care:** The pin sites are typically covered with a sterile dressing. Instructions are provided for pin site care at home to prevent infection. **Follow-Up:** Given that the Steinmann pins cross the physis (growth plates), it is essential to monitor the patient's growth and development over several years. This can involve: 1. **Short-term Follow-Up:** These visits focus on fracture healing, pin site condition, and early rehabilitation. They typically occur weeks to months after surgery. 2. **Medium-term Follow-Up:** These visits focus on the restoration of function and the early detection of any growth disturbances or deformities. They typically occur every few months to annually for the first few years after surgery. 3. **Long-term Follow-Up:** These visits focus on monitoring the growth of the femur and detecting any late deformities or discrepancies in leg length. They may continue annually until skeletal maturity. This long-term follow-up is vital for quality outcomes because: 1. It allows for early detection and management of potential complications, including infection, pin migration, and non-union. 2. Growth disturbances can occur years after injury, so regular monitoring of the growth plates helps identify and manage such issues early. 3. It provides an opportunity to assess and manage any functional issues, facilitating appropriate interventions such as physiotherapy or additional surgery. 4. Psychological aspects, including the patient's perception of their recovery, can be monitored and managed over time.
Orthopaedic implants used: Steinmann pins at a cost of about $2.67
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities




Article viewed 795 times
30 Jun 2023
Add to Bookmarks
Full Citation
Cite this article:
David Bennett. (2023). A tale of 2 pins. Journal of Orthopaedic Surgery and Traumatology. Case Report 21102224 Published Online Jun 30 2023.