Minimally invasive reduction of a posterolateral plateau "apple-bite" fracture
Score and Comment on this Case
Clinical Details
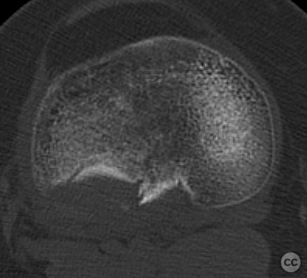
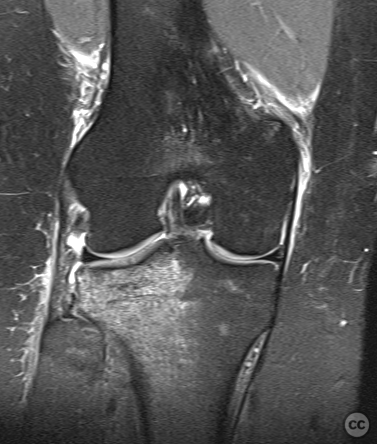
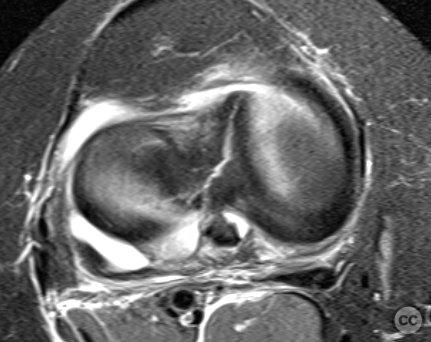
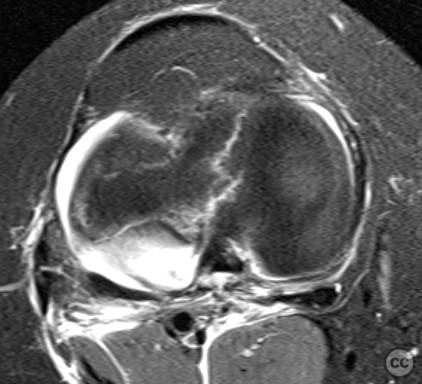
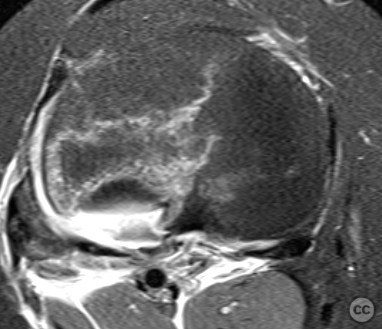
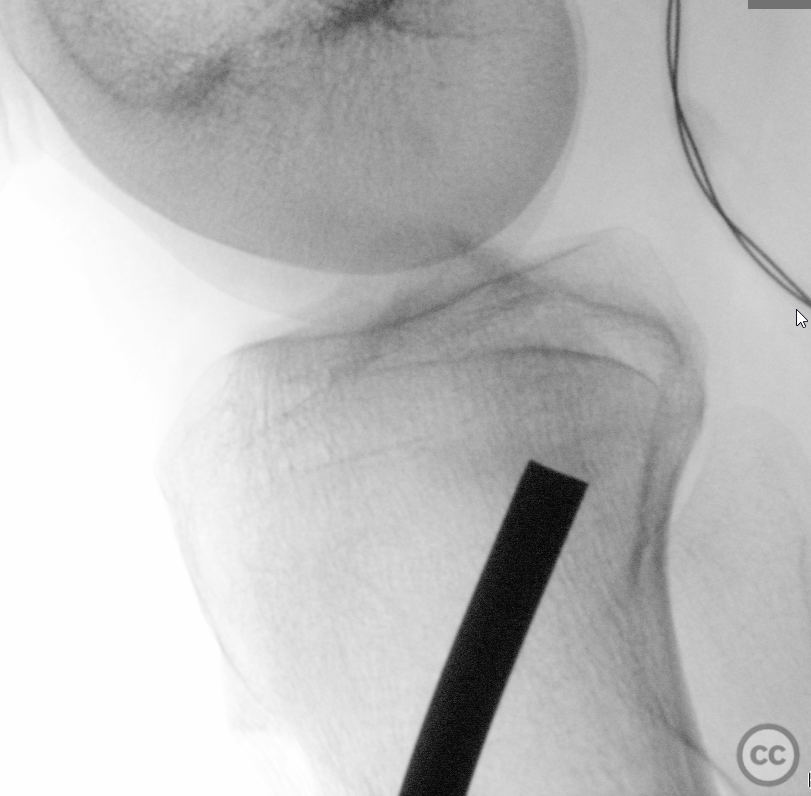
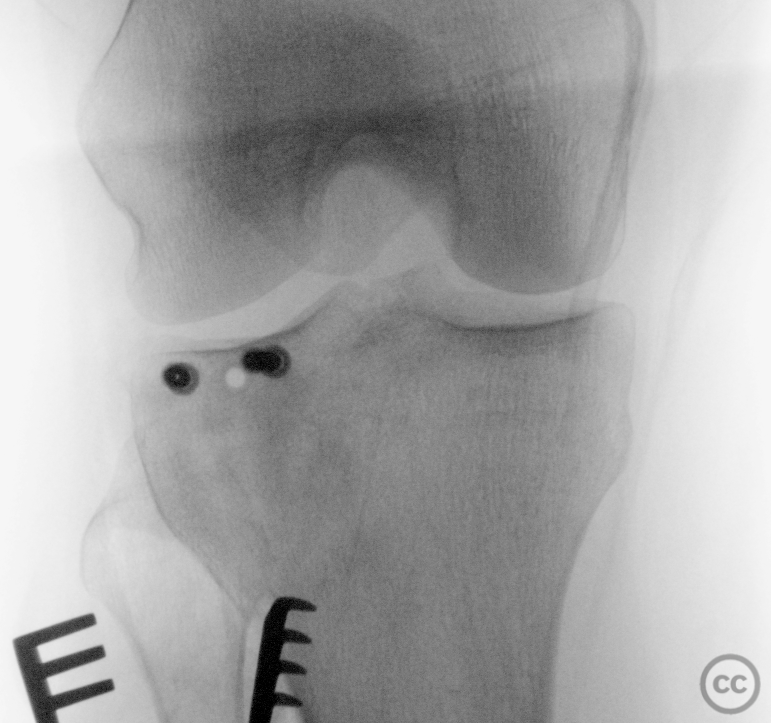
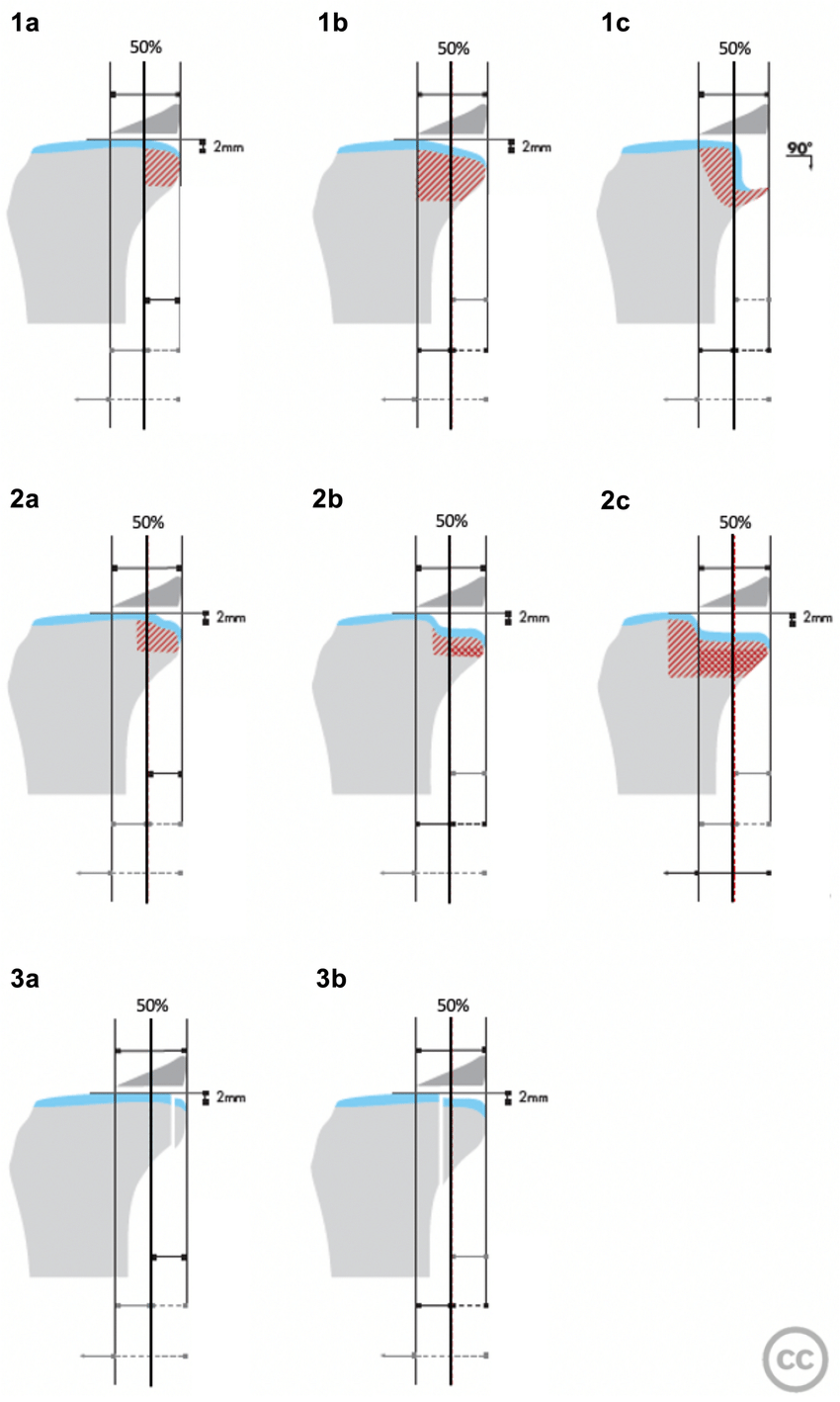
Clinical and radiological findings: A 34-year-old female presented after a fall from an e-bike with a clinically unclear injury to the right knee, Plain film imaging was inconclusive for specific acute bony injury, although a lipo-haemarthrosis is evident. A CT scan confirmed the diagnosis of a focally impacted posterolateral tibial plateau fracture, a classical "apple bite" configuration. Subsequent MRI excluded commonly associated injuries such as ACL rupture, meniscal tear, or femoral chondral impression injury.
Preoperative Plan
Planning remarks: The preoperative plan focused on minimally invasive restoration of posterolateral joint height to re-engage meniscus function.
Surgical Discussion
Patient positioning: The patient was positioned supine with the right leg over a carbon fiber roll at the distal thigh level. Fluoroscopy was used to confirm radiological access before sterile preparation and draping.
Anatomical surgical approach: A 5 cm curved incision was made over the lateral aspect of the proximal tibia, just distal to the joint line, curving over Gerdy's tubercle.
Operative remarks:Subcutaneous dissection identified the fibres of the iliotibial band and anterolateral fascia, which were split longitudinally. Blunt dissection of muscle fibers from the inferior aspect of Gerdy's tubercle allowed for a 10x10 mm osteotomy window. A curved bone tamp was inserted through this window to elevate the depressed posterolateral corner under multiplanar fluoroscopic guidance.
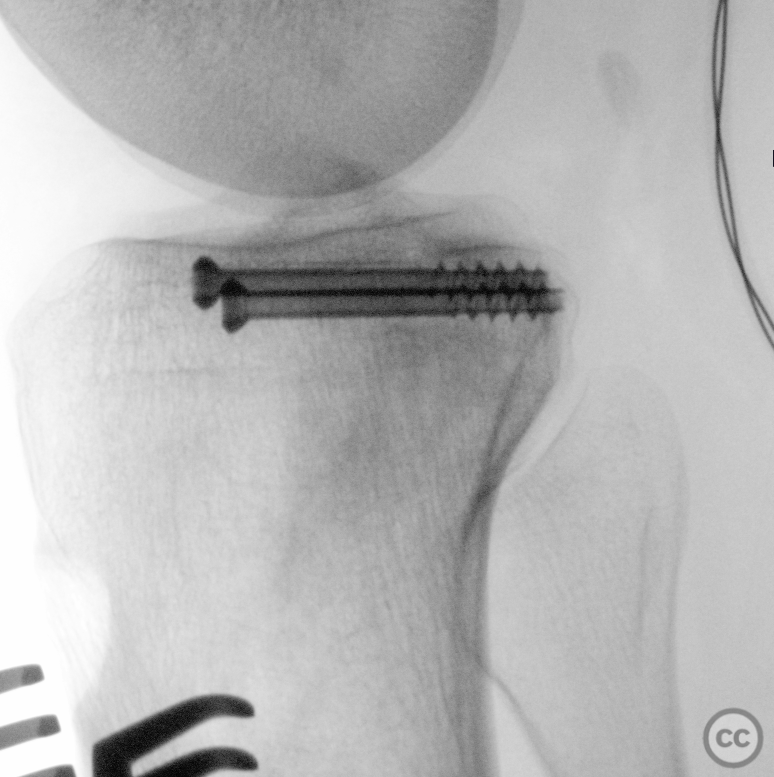
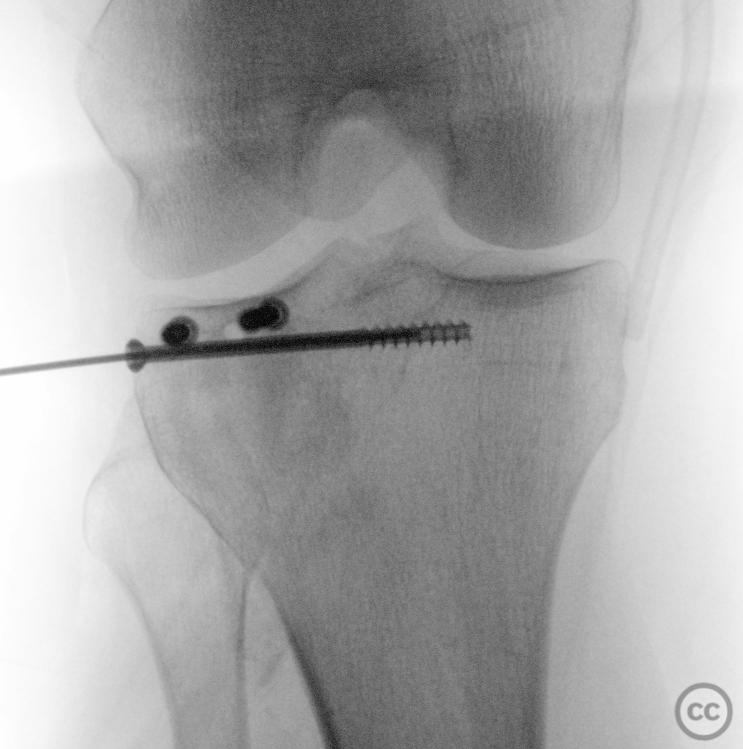
Anatomical reduction was achieved and confirmed under live fluoroscopy with dynamic demonstration of the zone of injury. Two 4.0 mm cannulated screws were placed anterior-posteriorly, with one screw repositioned for optimal fixation. A third jail-screw was introduced laterally as secondary buttress support. The defect in the tibial metaphysis was filled with beta-tricalcium phosphate (Vitoss) ceramic bone void filler, and the osteotomy window was closed with the existing hinged cortical flap.
Postoperative protocol: The postoperative protocol included non-weight bearing with free range of motion for 8 weeks, progressing to full weight bearing (FWB) by week 10 without the use of orthosis.
Orthopaedic implants used: 3x 4.0 mm cannulated screws - Vitoss ceramic bone void filler
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisThe literature consistently reports a strong correlation between posterolateral tibial plateau fractures and ACL injuries. In particular, Flury et al. report a significant association between higher-grade posterolateral tibial plateau impaction fractures (TPIF) and anterolateral complex injury, which correlates with poorer functional outcomes post-ACL reconstruction [1]. Korthaus et al. similarly highlight the prevalence of these fractures in the setting of ACL ruptures and their association with meniscal and medial collateral ligament injuries [2]. These findings are crucial as they suggest that the presence of a posterolateral apple bite fracture may be indicative of a more complex injury pattern requiring a comprehensive management approach.
Bernholt et al. provide insight into the incidence of posterolateral tibial plateau and lateral femoral condyle impaction fractures in ACL tears, emphasizing the increased association with lateral meniscus posterior horn root tears [3]. This study, along with that of Menzdorf et al., highlights the importance of a thorough assessment of the meniscus and collateral ligaments in cases of ACL injury with concomitant posterolateral tibial plateau fractures [4].
The biomechanical study by Milinkovic et al. provides a unique perspective on the impact of high-grade posterolateral tibial plateau fractures on knee kinematics, specifically noting increased translational and anterolateral rotational instability in ACL-deficient knees [5]. This underscores the mechanical significance of the posterolateral tibial plateau in knee stability and function.
Clinical management strategies for these injuries vary. Solomon et al. suggest that direct posterolateral transfibular approaches to these fractures yield better outcomes than indirect anterolateral approaches [6]. Li et al. advocate for single-stage arthroscopic-assisted surgery for combined anteromedial tibial plateau fracture with posterolateral corner injury, claiming good outcomes [7]. These surgical approaches are supported by the work of Menzdorf et al. and Frosch et al., who offer insights into the surgical management of posterolateral tibial plateau fractures with ACL injuries [4, 8].
In summary, the existing literature suggests that 'apple bite' posterolateral tibial plateau fractures are frequently associated with ACL injuries and meniscal instabilities, with higher-grade fractures correlating with more severe concomitant injuries and worse functional outcomes. Surgical approaches to these fractures should be carefully chosen based on the specific fracture pattern and associated soft tissue injuries to optimize patient outcomes
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities


















Article viewed 930 times
14 Feb 2024
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2024). Minimally invasive reduction of a posterolateral plateau "apple-bite" fracture. Journal of Orthopaedic Surgery and Traumatology. Case Report 24583198 Published Online Feb 14 2024.