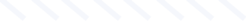
Rorabeck II Vancouver C inter-implant periprosthetic femur fracture
Score and Comment on this Case
Clinical Details
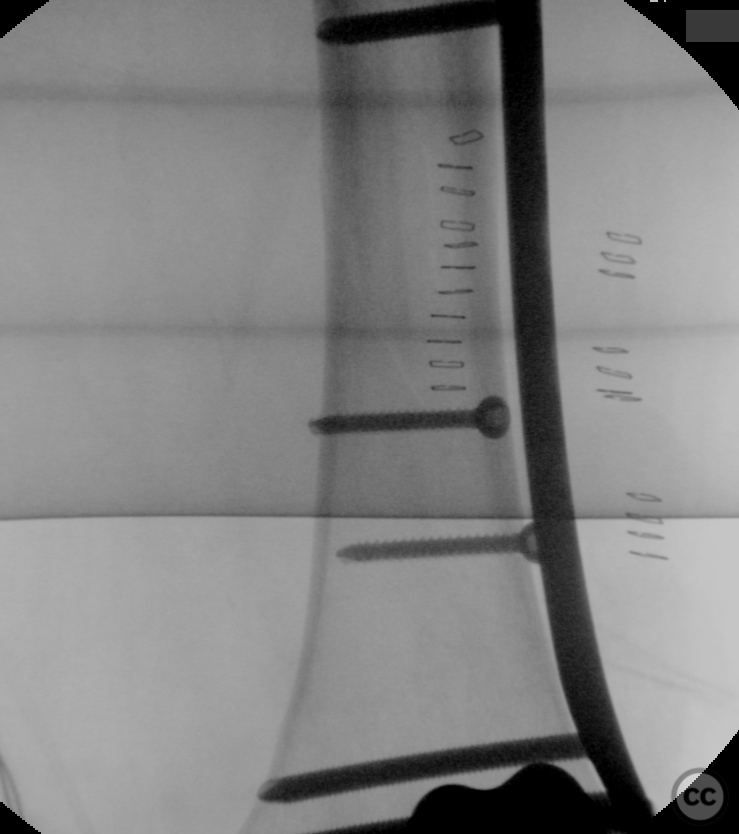
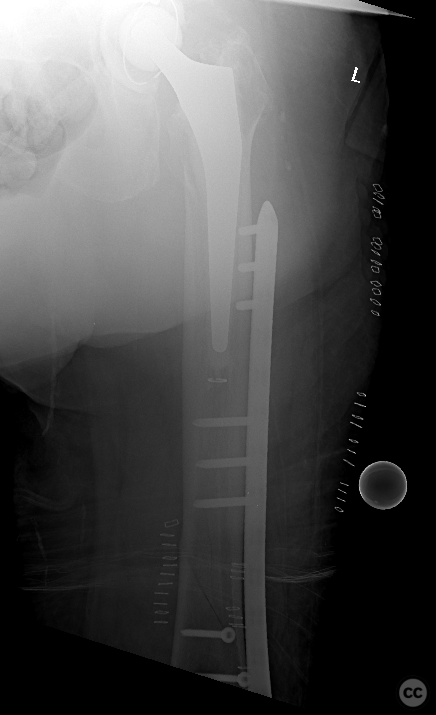
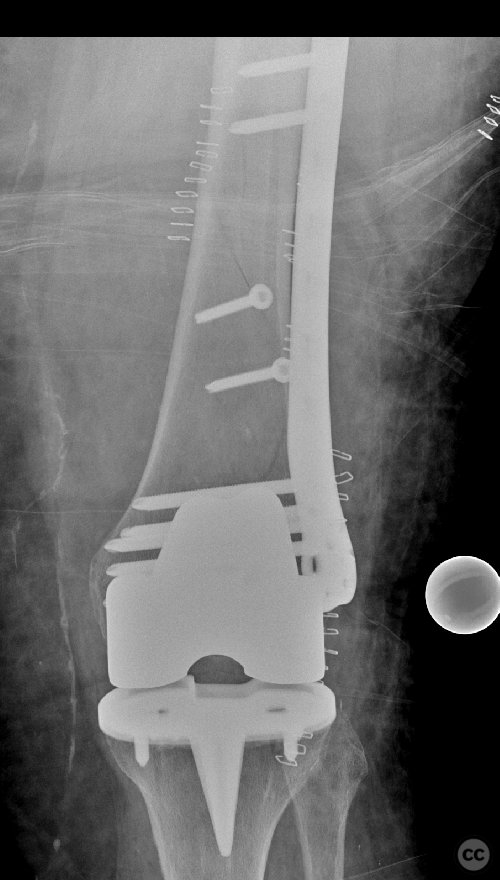
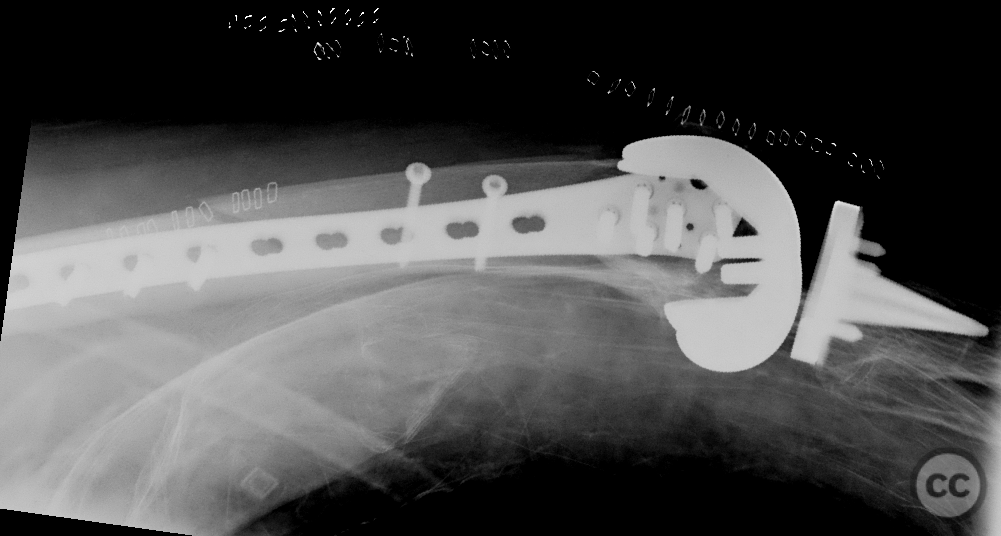
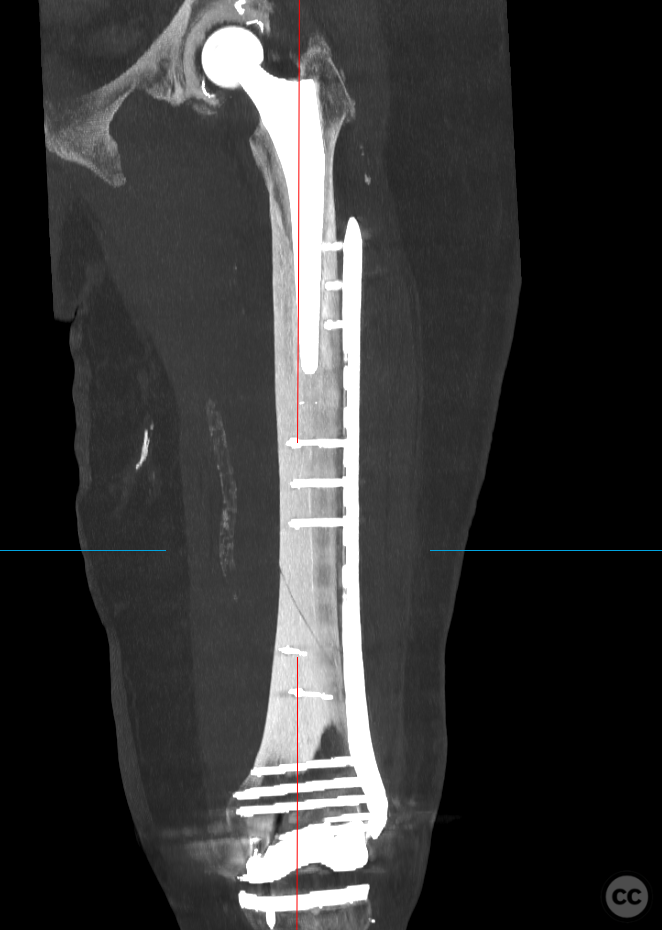
Clinical and radiological findings: An 82-year-old patient experienced a mechanical slip and fall at home, resulting in a closed injury with intact neurovascular status. The patient, who was independent in activities of daily living (ADLs) but had moderate mobility requiring the use of a walker, presented with a spiral inter-prosthesis femur fracture located between a cemented total hip and total knee prosthesis on the ipsilateral side. Radiographs revealed Rorabeck II Vancouver C long-spiral inter-implant periprosthetic fracture.
Preoperative Plan
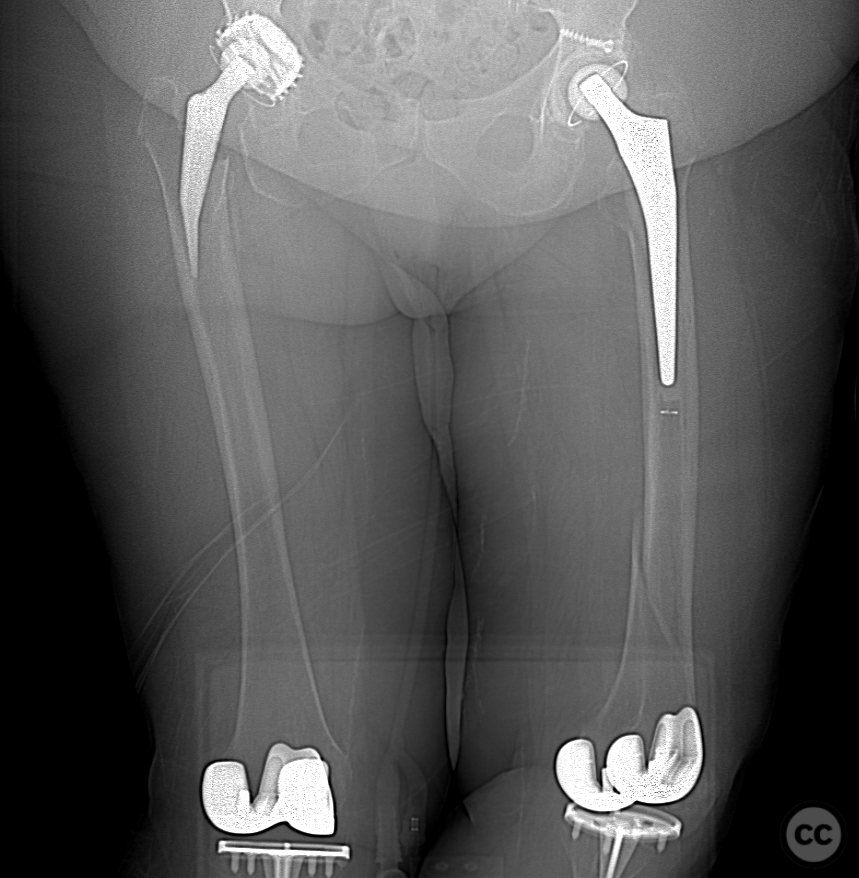
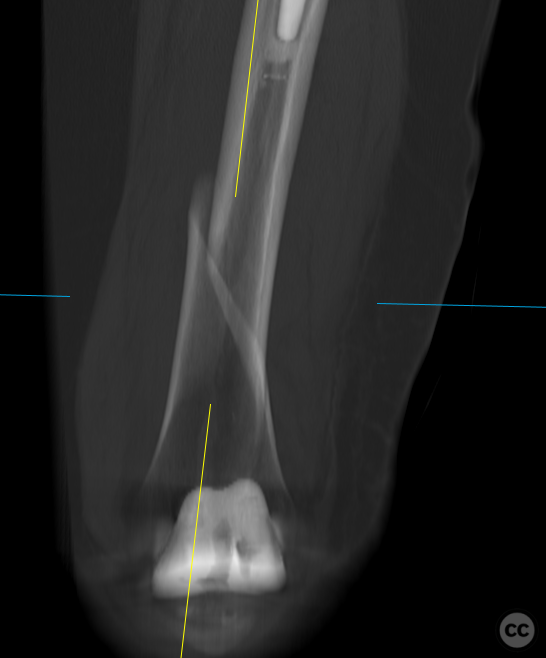
Planning remarks: Given the presence of adjacent prostheses, planning focused on achieving stable fixation while minimizing secondary trauma to the surrounding tissue. The submuscular Less Invasive Stabilization System (LISS) plate using Minimally Invasive Plate Osteosynthesis (MIPO) technique was planned. Preoperative imaging was reviewed to plan plate length and screw placement avoiding interference with existing implants and ensuring adequate overlap between the plate and distal femoral stem component as per literature recommendations.
Surgical Discussion
Patient positioning: The patient was positioned supine on the operating table with a bump placed under the distal thigh to facilitate access to the lateral aspect of the femur.
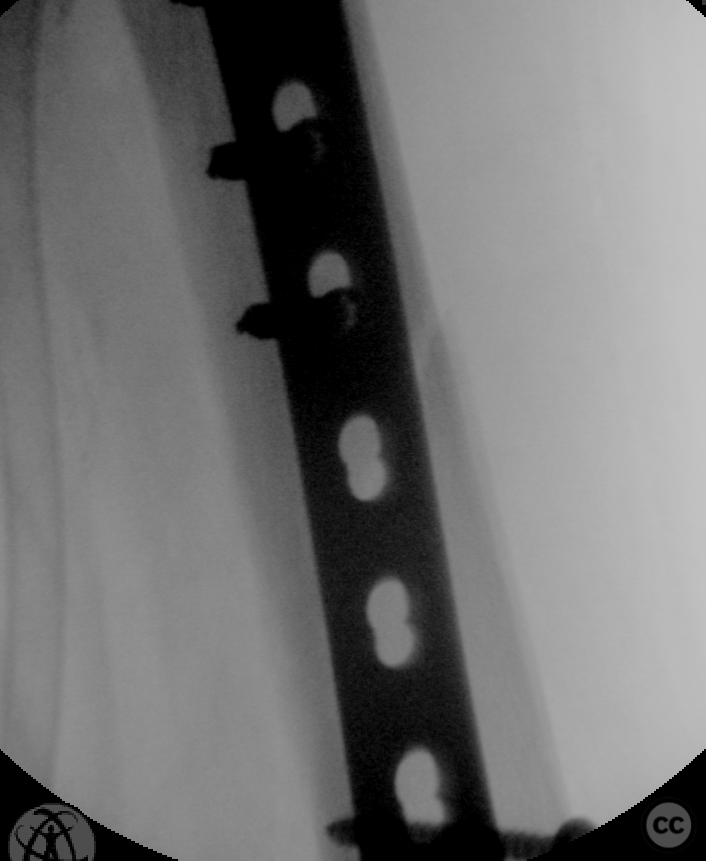
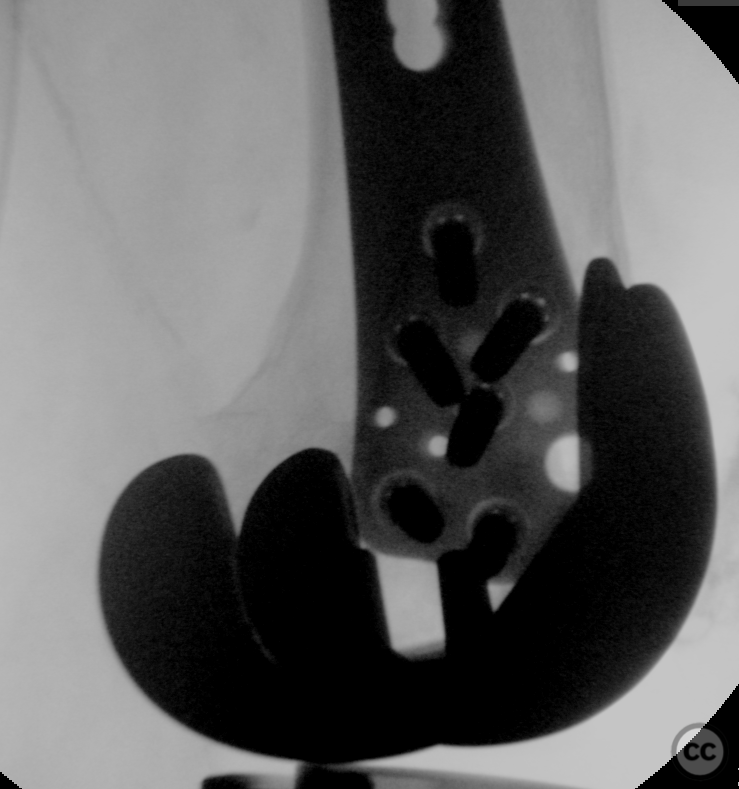
Anatomical surgical approach: A minimally invasive approach was utilized starting with a distal incision through the iliotibial band and vastus lateralis overlying the lateral femoral condyle for plate insertion. A subvastus dissection allowed for submuscular passage of the LISS plate along the lateral aspect of the femur.
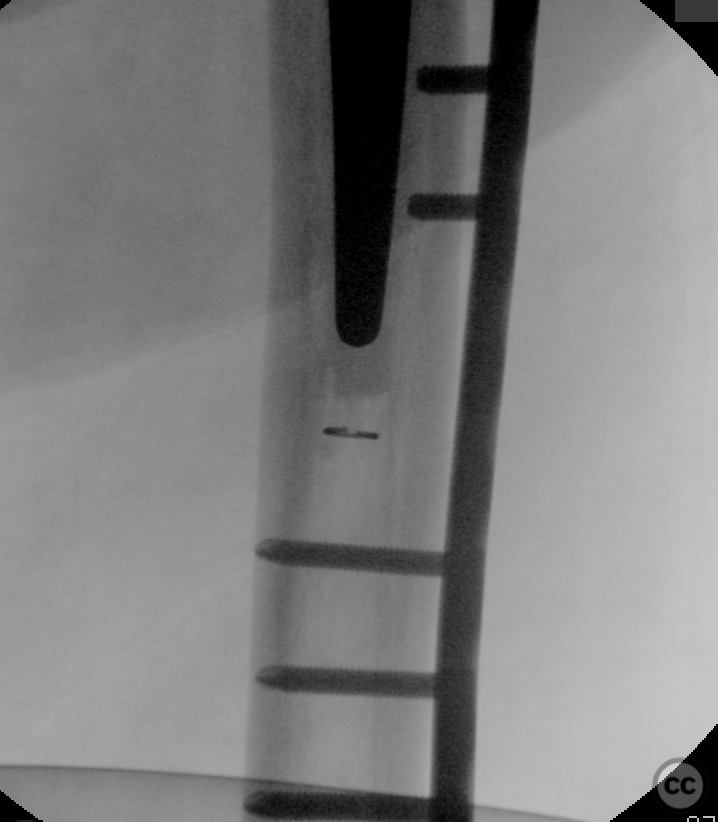
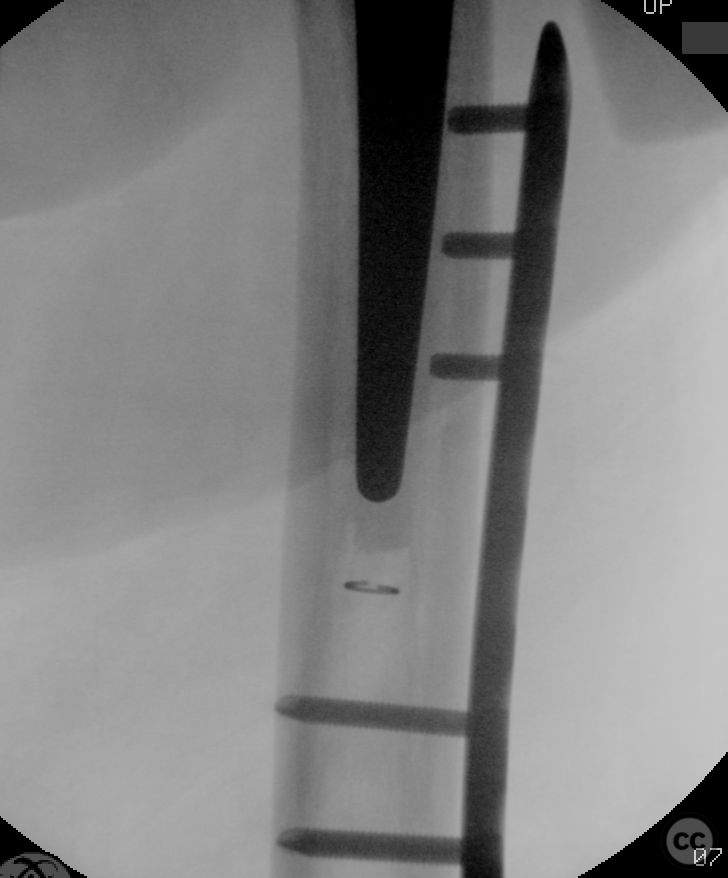
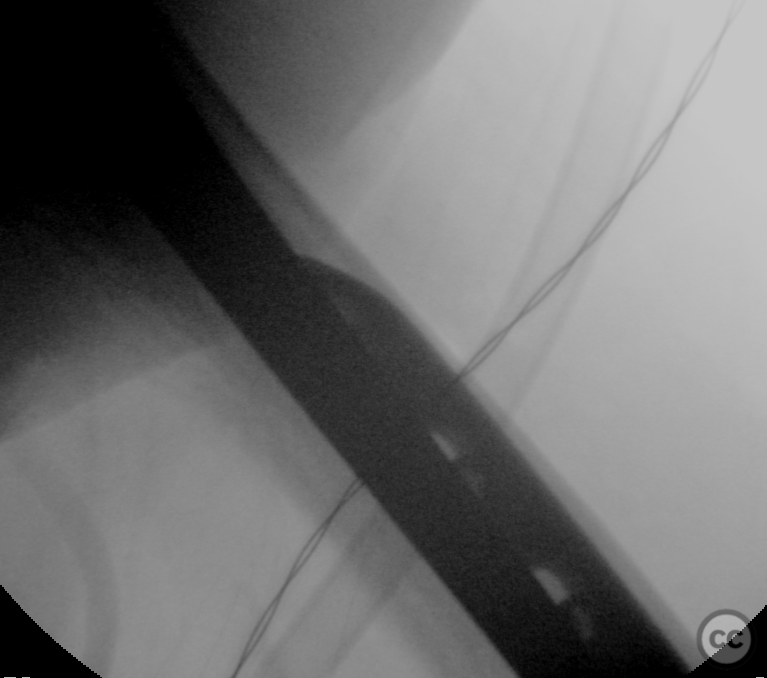
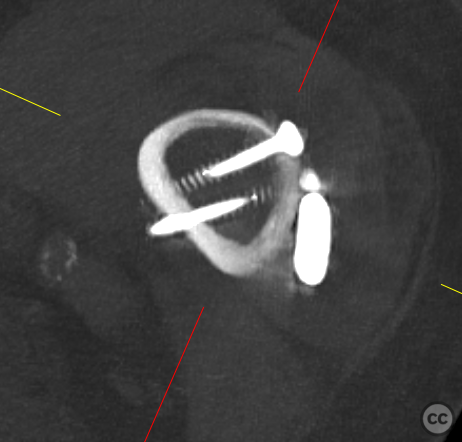
Operative remarks:Closed reduction under axial traction facilitated provisional fixation using two percutaneous lag screws, achieving near-anatomic reduction. I feel that 2 screws may provide sufficient additional axial stability to facilitate weight bearing through the fracture, without unduly reducing med-lat strain (an artefact of a laterally positioned plate, putting the fracture into bending) thus retaining a relative stability construct. Following screw placement, a LISS plate was inserted submuscularly through a minimally invasive approach, initially secured proximally and distally using K-wires under fluoroscopic guidance. Definitive screw fixation was then achieved through stab incisions guided by fluoroscopy, ensuring placement away from the proximal prosthetic stem to mitigate stress concentration risk. Overlap of more than 6cm between plate and distal femoral stem component adhered to biomechanical study recommendations for reducing inter-prosthetic strain.
Postoperative protocol: The patient was advised patial weight-bearing initially due to the limitations of single lateral off-axis plate stability. Gradual progression towards full weight-bearing as tolerated was guided by clinical assessment and radiographic evidence of retention of reduction over a 2-6 week period.
Orthopaedic implants used: LISS Plate - Percutaneous Lag Screws - K-Wires (for temporary stabilization during plate positioning)
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisBiomechanics concerning plate-stem overlap aims to ensure stability and prevent stress risers that could lead to implant failure or refracture [1-3]. The biomechanical study by Walcher et al. (2016) utilized composite femurs with cemented hip stems and applied distal femoral plates at varying distances from the stem tip [1]. Their findings indicated that strain on the bone increased with decreasing overlap or gap between plate and stem, suggesting that closer proximity may predispose to higher stress concentrations. They recommended at least 6 cm of minimal gap or overlap in osteoporotic bone models to avoid creating stress risers. Kempthorne et al. (2018) examined different configurations using composite bones fitted with cemented stems overlapped by lateral plates [2]. Their results also emphasized lower strain levels when there was sufficient proximal extension of the plate past the tip of the stem—specifically two shaft diameters—which corresponds roughly to approximately 6 cm depending on bone size. Constructs without overlap or those with small gaps demonstrated significantly higher strains leading to lower forces required for fracture under torsional and lateral bending loads. Similarly, Kubiak et al. (2015) analyzed cortical strain and load-to-failure relationships between locked compression plating constructs overlapping cemented stems [3]. Their data showed reduced cortical strain as constructs transitioned from an 8 cm gap between plate end and stem tip towards overlapped configurations, corroborating earlier findings regarding optimal construct length for mitigating stress concentration effects. Collectively, these studies suggest that there is an optimal zone where plate fixation should either sufficiently overlap or be spaced away from a pre-existing femoral stem within certain limits—too close may create high stresses while too far might not provide adequate support against loading forces experienced during normal activities or falls post-surgery. In summary, based upon current biomechanical evidence available through these analyses: - There appears to be consensus recommending an approximate distance of at least two shaft diameters—or around 6 cm—as being beneficial for reducing inter-prosthetic strain. - Overlapping constructs have shown reduced cortical strains compared with non-overlapping ones. - A minimum safe distance should be maintained between plate end and prosthesis tip to minimize risk factors associated with subsequent fractures due to elevated local stresses. These conclusions serve as guidelines derived from simulated conditions which must be carefully interpreted within clinical context considering patient-specific factors such as bone quality, activity level, weight-bearing status among others before translating into surgical practice decisions.
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant
Industry Sponsership
contact us for advertising opportunities












Article viewed 1016 times
15 Dec 2023
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2023). Rorabeck II Vancouver C inter-implant periprosthetic femur fracture. Journal of Orthopaedic Surgery and Traumatology. Case Report 27452888 Published Online Dec 15 2023.