Combined distal 1/3 tibia fracture with SAD bimalleolar ankle fracture
Score and Comment on this Case
Clinical Details
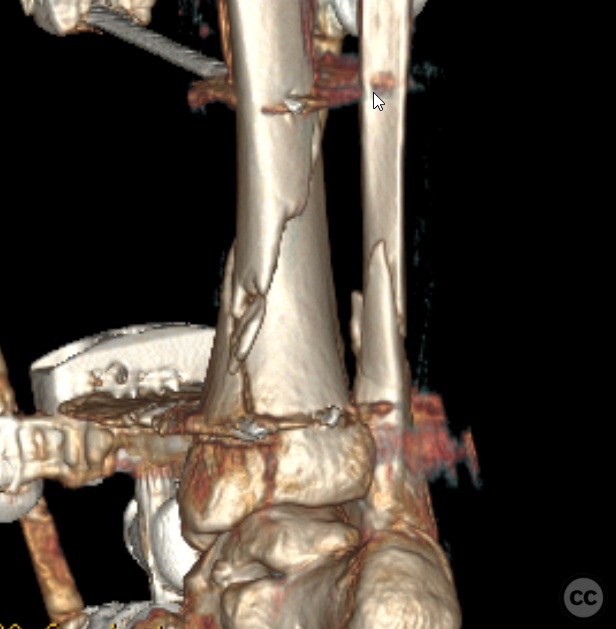
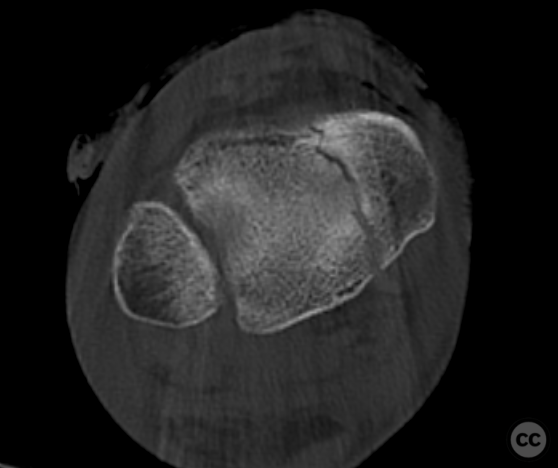
Clinical and radiological findings: A mixed bag injury sustained by a middle-aged female motor vehicle accident. This was a GA type 2 open injury which was provisionally debrided and stabilised in an external fixator. Definitive fixations was performed around 7 to 10 days post injury following consolidation of soft tissue. Initially categorised as a simple distal tibial spiral fracture with concomitant fibula fracture preoperative CT planning demonstrated plafond extension together with a Weber A bony avulsion of the distal fibula. This is more in fitting with two isolated injuries: that of the tibial shaft and fibula at the same level and a supination adduction ankle injury resulting in vertical shear of the medial malleolus and avulsion of the fibula apex. This is a little different to the classical occult posterior malleolus fracture associated with distal tibial spiral fractures (for which there is good evidence for the use of CT scanning to plan plafond stabilisation0.
Preoperative Plan
Planning remarks: Although potentially nailable I opted for minimally invasive plate fixation of this fracture. Plate fixation provided the advantage of anatomical reduction with lagscrew compression of the tibial spiral fracture. Similarly anatomical reduction and lagscrew fixation of the tibial plafond could be simultaneously performed.
Surgical Discussion
Patient positioning: Supine
Anatomical surgical approach: Minimally invasive medial, standard lateral.
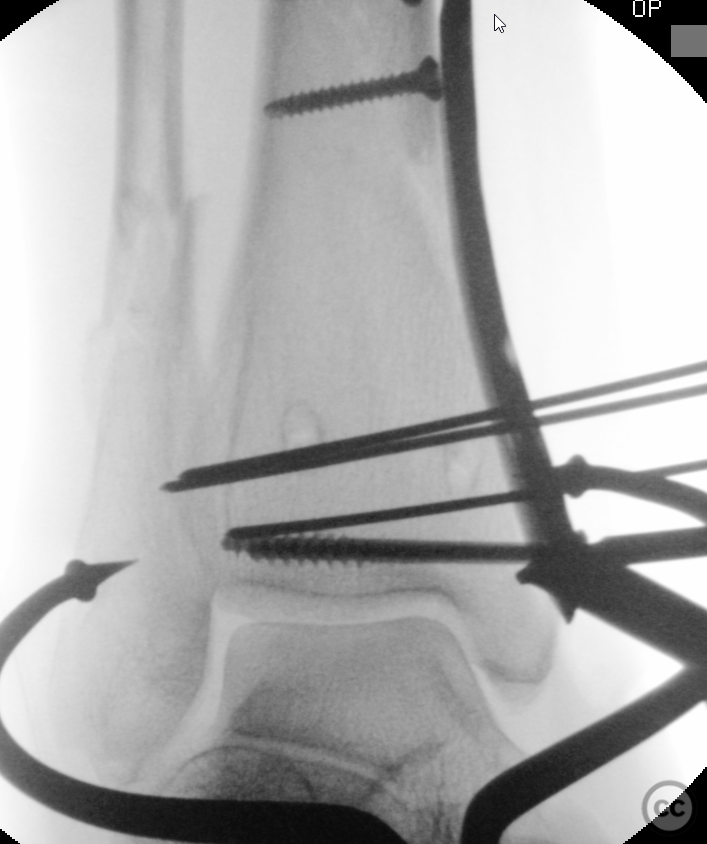
Operative remarks:Following the pre-operative plan distal lagging was achieved through the distal aspect of the medial tibial plate optimising the use of hardware. Proximal plate fixation was done percutaneously. The fluoroscopy imaging of lag screw closure of the plafond fracture gap is always satisfying. Lateral reduction and fixation of the high fibula fracture was unremarkable. Given the SAD distal avulsion, suture anchor fixation of the lateral ligamentous structures was done. This suture anchor is evident at the tip of the lateral fibula plate. This patient will be managed with partial weight bearing progressing to full weight bearing after 6 weeks.
Postoperative protocol: TWB progressing to PWB over 6W. FWB following 6week review. Follow-up XR provided is at 12M post op.
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities












Article viewed 1478 times
21 Dec 2022
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2022). Combined distal 1/3 tibia fracture with SAD bimalleolar ankle fracture. Journal of Orthopaedic Surgery and Traumatology. Case Report 27994453 Published Online Dec 21 2022.