Open Medial Malleolus Fracture-Dislocation with Tibial Pilon and Lateral Malleolus Fractures
Score and Comment on this Case
Clinical Details
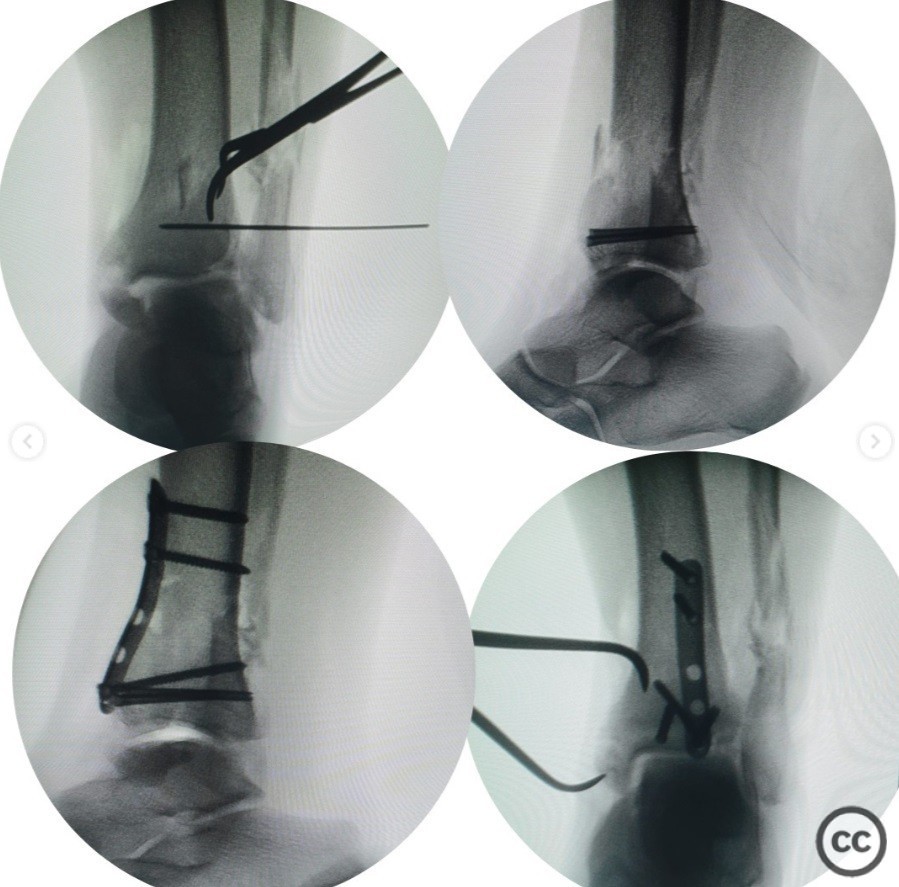
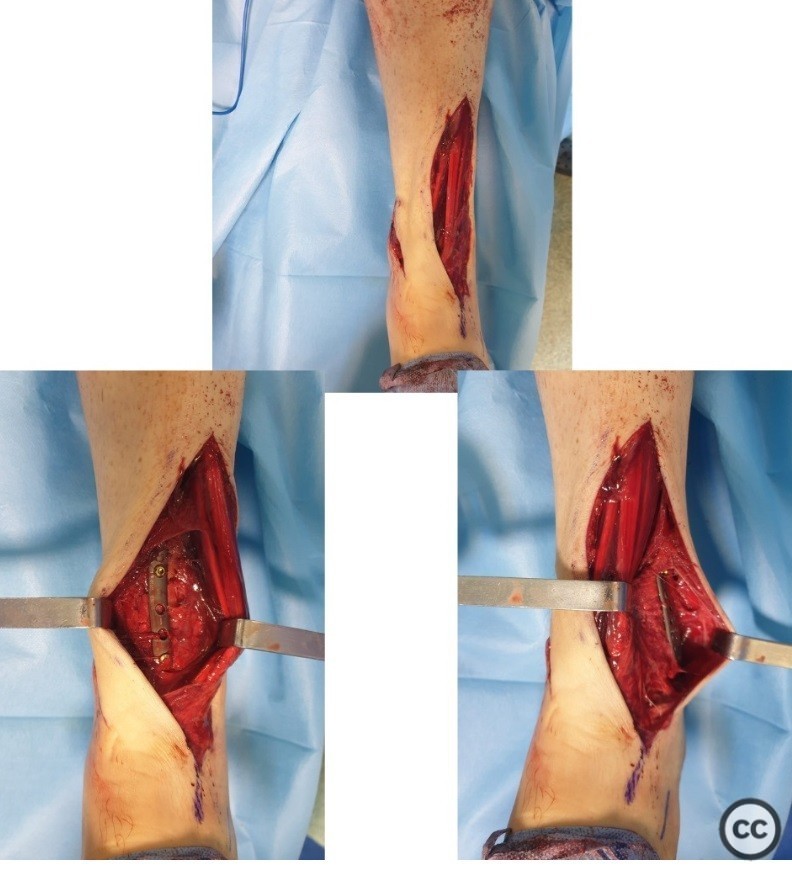
Clinical and radiological findings: A 57-year-old male presented to the emergency department following a fall from a height, sustaining a medial malleolus type 2 open fracture-dislocation, a tibial pilon fracture, and a lateral malleolus fracture. The neurovascular examination was normal. The patient arrived at the emergency room within 30 minutes post-injury. Prophylactic antibiotics were administered promptly. Initial wound debridement and closure were performed in the emergency department, followed by a CT scan prior to urgent surgical intervention.
Preoperative Plan
Planning remarks: The preoperative plan involved an anterolateral approach to address the tibial pilon fracture and lateral malleolus fracture, with a separate approach for the medial malleolus. Definitive fixation was planned during the initial surgical session due to the patient's favorable condition and soft tissue status.
Surgical Discussion
Patient positioning: Supine position on the operating table.
Anatomical surgical approach: Slightly lateral anterolateral incision was made to access the anterolateral pilon fracture and lateral malleolus. The anterolateral pilon fracture was visualized and reduced using a Weber clamp, followed by fixation with two 4mm headless compression screws. An antiglide plate was applied using a 1/3 semitubular plate. The medial malleolus was accessed separately and fixed with two 4.5mm headless compression screws. Through the anterolateral incision, the lateral malleolus fracture was exposed proximally and distally, preserving comminuted fragments, and osteosynthesis was performed using a plate. Syndesmosis fixed with one syndesmosis screw.
Operative remarks:The decision to proceed with definitive fixation in the initial session was based on the patient's non-smoking status, absence of diabetes mellitus, good overall condition, and favorable soft tissue condition. The use of headless compression screws allowed for stable fixation of the fractures while minimizing soft tissue disruption.
Postoperative protocol: Partial weight-bearing was initiated at 6 weeks postoperatively, progressing to full weight-bearing as tolerated by 12 weeks.
Follow up: Not specified
Orthopaedic implants used: Two 4mm headless compression screws, 1/3 semitubular plate, distal fibula anatomic plate, two 4.5mm headless compression screws, syndesmosis screw.
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities







Article viewed 33 times
16 Apr 2025
Add to Bookmarks
Full Citation
Cite this article:
Gumusgoz M. (2025). Open Medial Malleolus Fracture-Dislocation with Tibial Pilon and Lateral Malleolus Fractures. Journal of Orthopaedic Surgery and Traumatology. Case Report 30585442 Published Online Apr 16 2025.