Revision Osteosynthesis for Malunited Midshaft Radius Fracture
Score and Comment on this Case
Clinical Details
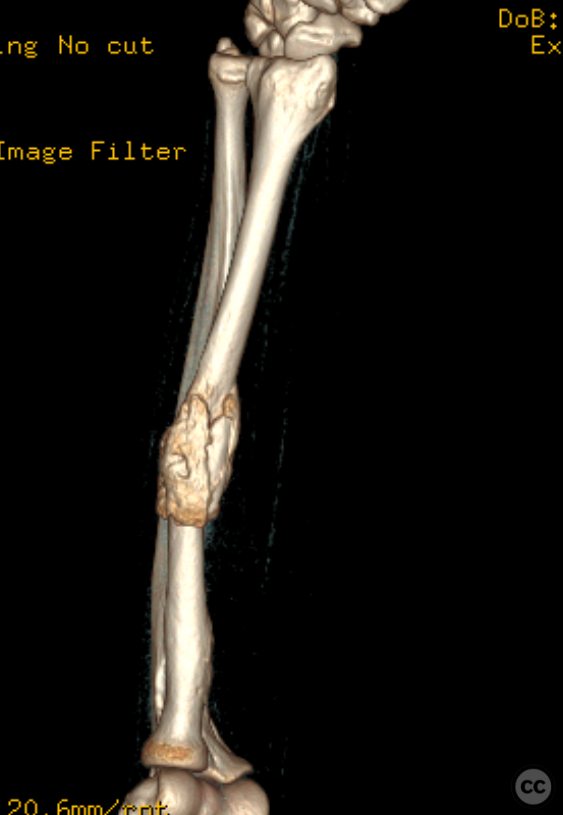
Clinical and radiological findings: A 38-year-old male presented with a midshaft radius fracture sustained from a bicycle fall. Initial conservative management was employed. At 5 weeks, radiographs and clinical examination revealed an angular malunion with an apex-posterior deformity and 30 degrees of limited pronation/supination.
Preoperative Plan
Planning remarks: The preoperative plan involved revision surgery using 3D planning to correct the malunion. Approximately 30deg of mal-rotation was identified along the long axis of the radius
Surgical Discussion
Patient positioning: The patient was positioned supine on the operating table with the arm placed on an arm table.
Anatomical surgical approach: Henry's approach - A longitudinal incision was made along the border between the flexor carpi radialis and brachioradialis muscles in the mid-forearm. The radial neurovascular bundle was identified and protected. The pronator teres muscle was released from its radial attachment to expose the fracture site for osteotomy and plate osteosynthesis.
Operative remarks:Intraoperatively, an osteotomy was performed to derotate the malalignment correct the angular malunion. Careful debridement of callus and precise anatomical reduction were achieved utilising the ridge of the interosseous membrane as a rotational landmark. A 3.5mm locking compression plate (LCP) was provisionally fixed with K-wires, followed by definitive fixation with cortical screws using dynamic compression technique. Fluoroscopic imaging confirmed optimal plate placement and restoration of the radial bow.
Postoperative protocol: Postoperative rehabilitation protocol included early functional physiotherapy without load-bearing restrictions. No cast immobilization was deemed necessary; however, a symptomatic sling was provided for comfort during daily activities and nighttime support if needed.
Orthopaedic implants used: Eight-hole 3.5mm Synthes Locking Compression Plate
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisCorrective osteotomy of the radius following fracture nonunion is a complex procedure that requires meticulous preoperative planning and precise intraoperative execution to restore normal anatomy and function [1-3]. The fundamental themes emerging from the literature emphasize the importance of detailed imaging analysis, three-dimensional (3D) simulation, patient-specific instrumentation, and advanced intraoperative visualization techniques.
The use of 3D imaging has revolutionized preoperative planning by allowing surgeons to appreciate deformities in all planes accurately. This technology facilitates the simulation of corrective procedures using mirrored images from the unaffected limb as templates [3]. Bauer et al. demonstrated that patient-specific surgical guides manufactured based on such simulations could lead to successful outcomes in children with forearm deformities [3]. Their study showed significant improvements in forearm rotation arc postoperatively without any loss of range motion when using these custom guides.
Yoshii et al.'s research further supports technological advancements by introducing an image fusion system combining 3D preoperative plans with real-time fluoroscopy during surgery [1]. Their findings suggest improved reproducibility when utilizing this image fusion system compared to traditional methods without it. Specifically, they reported smaller discrepancies between planned corrections versus actual post-operative results at specific anatomical reference points when using their system.
Wada et al.’s article provides a step-by-step technique for simultaneous radial closing-wedge and ulnar shortening osteotomies aimed at treating malunions specifically involving distal radial fractures [2]. They underscored critical steps such as restoring volar tilt angle within a specified range through radial osteotomy while correcting ulnar variance via ulnar shortening. Although they did not utilize 3D printing or image fusion technologies directly mentioned in other studies reviewed here, their emphasis was on achieving precise correction through careful operative technique supported by fluoroscopic evaluation.
Collectively, these articles highlight several key considerations for planning corrective osteotomies:
1. Detailed Imaging: Preoperative imaging must be comprehensive enough to allow full appreciation of deformity. 2. Simulated Planning: Utilizing computer software aids in simulating potential corrections based on mirror images or other reconstruction algorithms. 3. Patient-Specific Instrumentation: Custom guides can ensure accurate translation from plan to surgical execution. 4. Intraoperative Visualization: Advanced systems like image fusion can enhance accuracy during surgery by superimposing virtual plans onto live fluoroscopic images. 5. Surgical Technique: Even with technological aids, meticulous surgical technique remains crucial; this includes respecting anatomical landmarks, managing soft tissues carefully, ensuring stable fixation post-osteotomy.
In conclusion, while each study contributes valuable insights into different aspects or techniques involved in corrective osteotomy for radius fracture nonunion—the integration of advanced imaging modalities coupled with patient-specific instruments appears essential for optimizing outcomes—this synthesis underscores an evolving paradigm shift towards precision medicine even within orthopedic surgery where individualized treatment strategies informed by high-fidelity simulations may become standard practice.
Author's Resources & References
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities








Article viewed 562 times
16 Feb 2024
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2024). Revision Osteosynthesis for Malunited Midshaft Radius Fracture. Journal of Orthopaedic Surgery and Traumatology. Case Report 30662241 Published Online Feb 16 2024.