O'Driscoll type II coronoid fracture dislocation with peristent PMRI
Score and Comment on this Case
Clinical Details
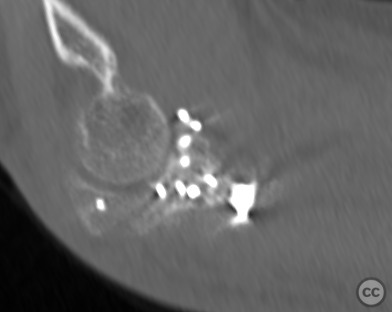
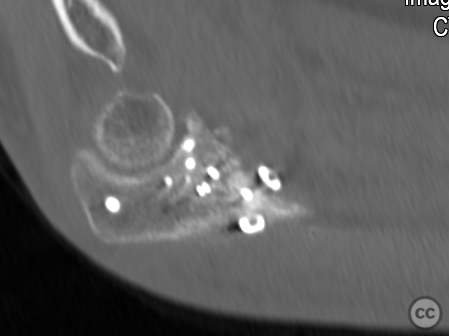
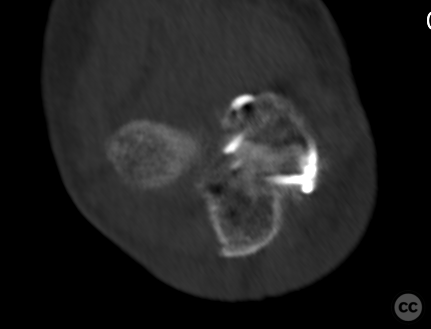
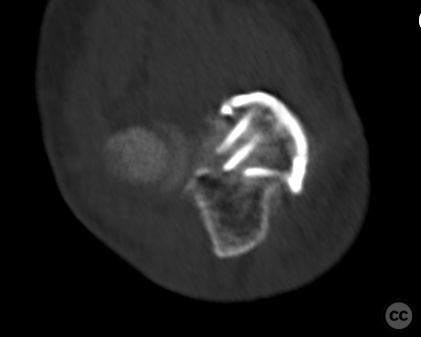
Clinical and radiological findings: A 68-year-old female experienced a fall on an outstretched arm while hiking recreationally in a forest, resulting in a closed elbow injury characterized by an apparent posterolateral dislocation. Radiological assessment revealed an intact radial head, displaced fragments of the coronoid process particularly affecting the anteromedial facet, and multiple small bony fragments around the medial collateral ligament (MCL) without involvement of the sublime tubercle. Post-reduction films showed perching of the trochlea into the coronoid defect, indicating a varus axial load force mechanism leading to primary failure of the anteromedial coronoid buttress and suggesting disruption of the MCL complex. This is not a terrible triad.
Preoperative Plan
Planning remarks: The operative plan involved addressing both medial and lateral aspects of the elbow to manage both the coronoid and suspected MCL complex disruption and lateral collateral ligament (LCL) injury following medial reconstruction. The approach aimed at restoring joint stability through direct repair and augmentation techniques, particularly focusing on reconstituting the integrity of both anterior and posterior bands of the MCL (aMCL and pMCL) as well as addressing any LCL injuries.
Surgical Discussion
Patient positioning: The patient was positioned supine with the arm placed on a mobile armboard, initially abducted and externally rotated to facilitate access to the medial side for initial exposure and repair.
Anatomical surgical approach: Medially, an FCU split approach was utilized to provide adequate visualization of the ulnar nerve early in the procedure, anticipating potential pMCL repair needs. This approach allowed direct access to address coronoid fractures and MCL complex disruptions effectively.
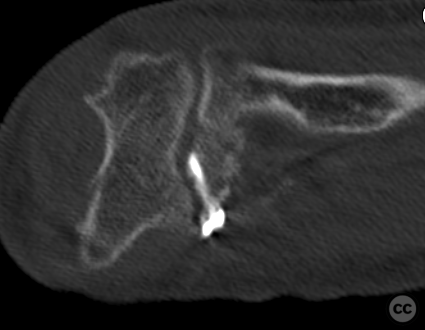
Operative remarks:Surgery commenced medially with identification and protection of the ulnar nerve followed by assessment of MCL complex integrity, revealing complete disruption including both aMCL and pMCL components. The naked sublime tubercle indicated complete distal loss of aMCL attachment. The coronoid fracture consisted of two large fragments which were initially reconstructed using PLLA pins before definitive fixation with a buttress plate.
Given the role of an intact pMCL in preventing postero-medial rotatory instability (PMRI) especially in cases involving coronoid injury, both aMCL and pMCL were reconstructed using an internal brace technique employing an ulnarcendobutton, 5.0mm and FastTak anchors loaded with FiberWire sutures.
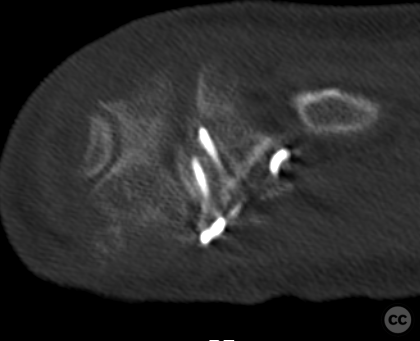
Subsequently, attention was turned laterally through an EDC splitting approach where complete humeral-sided avulsion of LCL was identified and repaired using a single 3.5mm FiberWire anchor.
Dynamic fluoroscopy confirmed restoration of joint stability under varus and valgus stress without evidence of PMRI or subluxation across full passive range-of-motion (PROM).
Postoperative protocol: Postoperatively, management included immobilization within a ROM brace set initially at 0-40-130 degrees for two weeks, followed by adjustments to 0-20-130 degrees for another two weeks before progressing to 0-0-130 degrees for four weeks aiming for achievement of a functional arc (90 degrees) by six-week mark.
Orthopaedic implants used: PLLA pins - Medartis coronoid buttress plate - Arthrex Biceps Endobutton - FastTak and 5.0mm anchors - FiberWire
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisThe posterior bundle of the medial collateral ligament (pMCL) plays a significant role in maintaining elbow stability, particularly against valgus stress and posteromedial rotatory instability (PMRI) [1][7]. PMRI is characterized by a specific pattern of osseous and soft tissue injuries that include anteromedial coronoid fractures with associated lateral collateral ligament complex (LCLC) injury [2]. It has been established that the integrity of the pMCL is essential for preventing PMRI as it resists valgus torque at various flexion angles [7]. Biomechanical analyses have demonstrated that isolated sectioning of the anterior bundle does not lead to complete dislocation until the pMCL is also compromised [7]. This suggests that while both bundles contribute to elbow stability, the pMCL serves as an important restraint against posterior dislocation across all flexion angles. Consequently, reconstruction techniques have evolved to address both anterior and posterior bundles when treating MCL injuries associated with instability or dislocation [7]. The relationship between contact pressures within the elbow joint structures during varus stress has been explored through biomechanical testing using cadaveric models. These studies reveal that intact specimens exhibit lower mean contact pressures compared to those with simulated PMRI injuries involving both LCLC tears and anteromedial subtype coronoid fractures combined with pMCL tears [1][8]. Notably, even without subluxation or joint incongruity caused by LCL lesions alone, increased contact pressures are observed in elbows affected only by anteromedial subtype coronoid fracture combined with pMCL tear compared to intact specimens [1]. Elbow stabilizers consist not only of ligamentous structures but also muscular components such as flexor-pronator muscles which actively contribute to valgus stability alongside passive stabilizers like MUCL[9]. Mechanoreceptors present within these ligaments suggest their role extends beyond mere mechanical support; they may provide proprioceptive feedback crucial for dynamic stabilization during movement[6]. In addressing failed lateral collateral ligament reconstructions – which often result in PMRI – preoperative risk factors concerning bony anatomy or soft tissue constraints must be considered along with operative factors such as tunnel placement or graft positioning[4]. Understanding these risk factors can inform preventative strategies. The interplay between different components contributing to elbow stability underscores a complex system where each element cannot be viewed in isolation. For instance, recent findings indicate that even parts typically not recognized as primary stabilizers – like the lateral part of distal triceps – play significant roles under certain conditions such as LCL-deficient elbows[8]. In summary, based on current literature spanning over two decades up till 2023[10], it's evident that while multiple elements contribute towards overall elbow stability against forces leading to PMRI including muscle loading effects from anconeus or triceps muscles[8], it's clear that preserving or restoring integrity specifically targeting pMCl remains paramount due its pivotal function against varus torque-induced instabilities across varying degrees elbow flexion.
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities


















Article viewed 987 times
26 Jan 2024
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2024). O'Driscoll type II coronoid fracture dislocation with peristent PMRI. Journal of Orthopaedic Surgery and Traumatology. Case Report 38119555 Published Online Jan 26 2024.