Nonunion of a reverse oblique proximal femur fracture
Score and Comment on this Case
Clinical Details
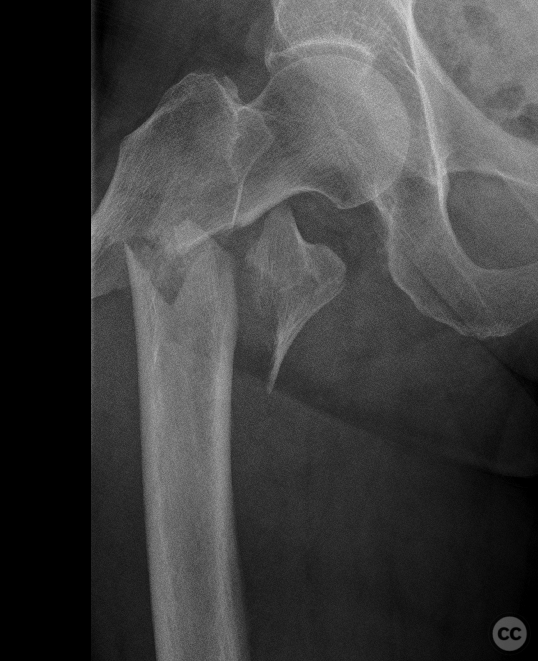
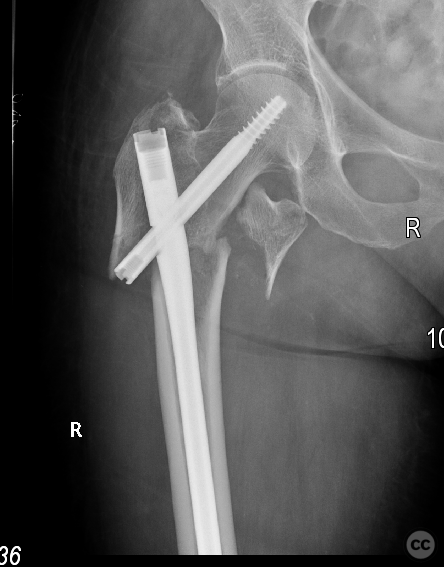
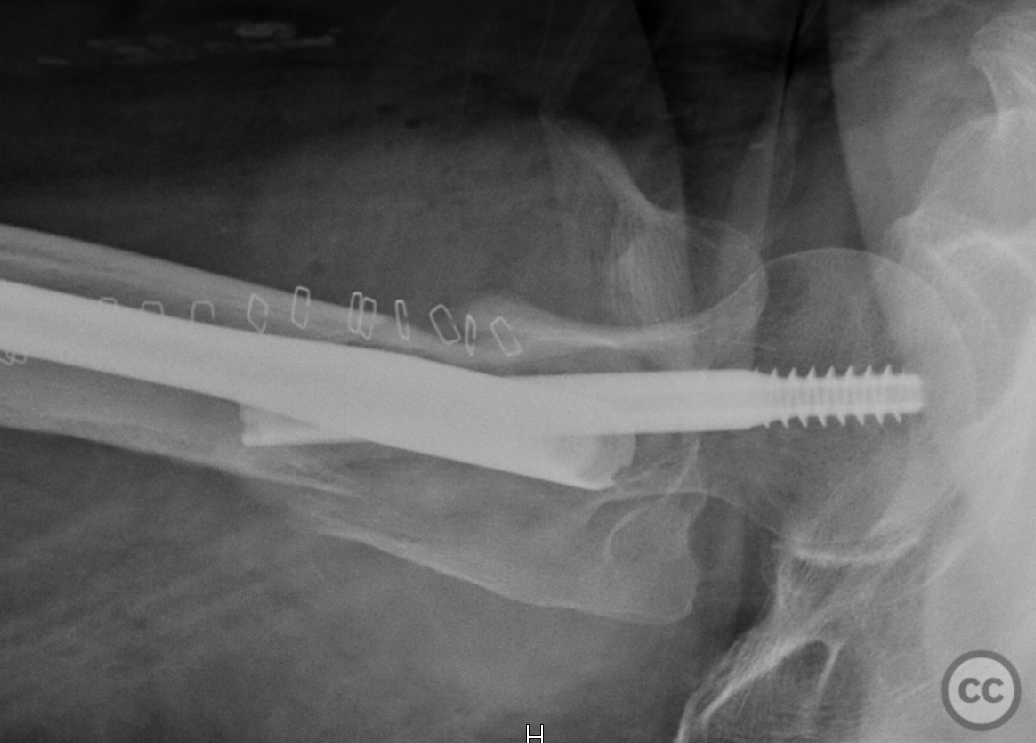
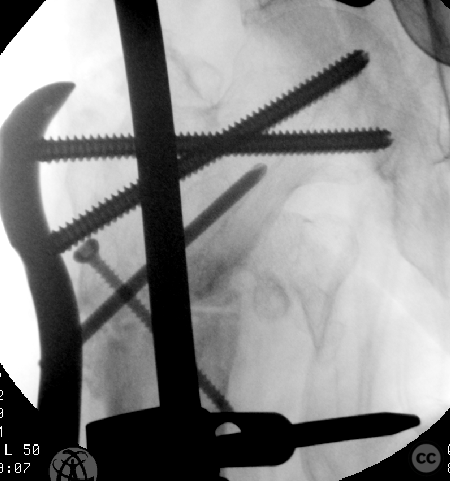
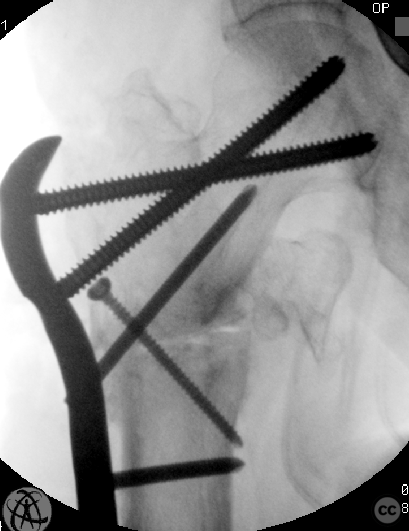
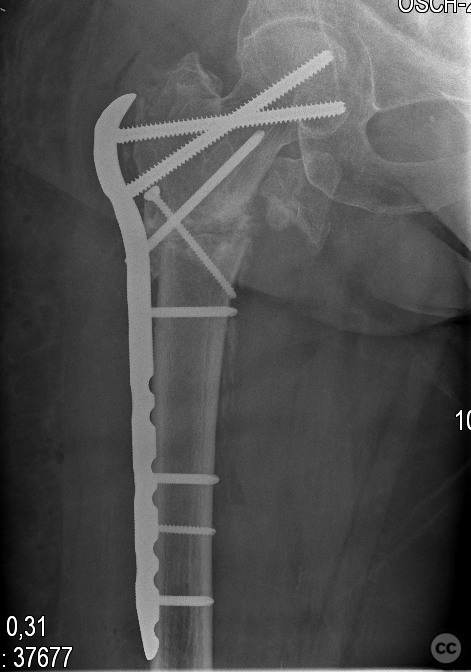
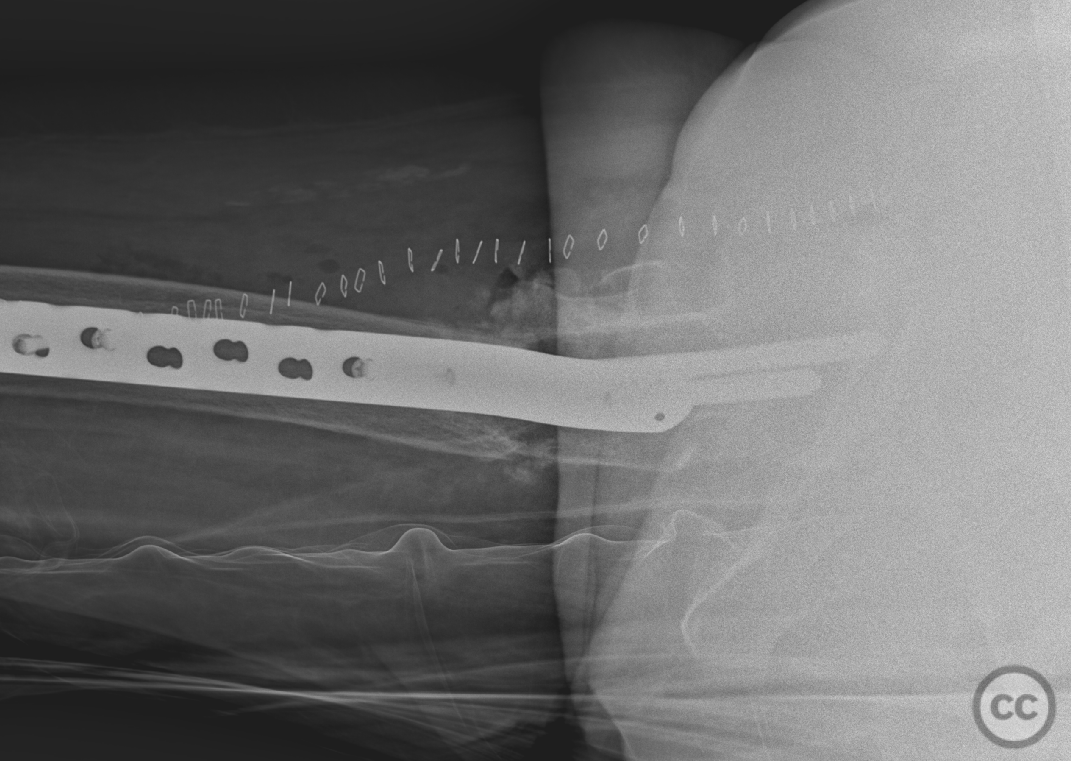
Clinical and radiological findings: Approximately 18 months prior, the patient sustained a reverse oblique (sub)trochanteric fracture of the right proximal femur. At that time, a closed reduction and gamma nail fixation were performed; however, the initial reduction was suboptimal, leading to early secondary varus displacement. The lateral aspect of the fracture demonstrated a tendency to kick laterally - which was anticipated given the fracture morphology and the initial fixation technique employed. Despite these challenges, the patient was able to bear full weight and unfortunately was lost to follow-up. Recently, the patient returned to the emergency department, reporting sudden inability to bear weight without any additional trauma. Imaging revealed a material failure of the gamma nail through the proximal screw hole, accompanied by a mature nonunion of the original fracture.
Preoperative Plan
Planning remarks: Revision with fixed angle femoral lockingplate
Surgical Discussion
Patient positioning: Traction table
Anatomical surgical approach: Direct lateral
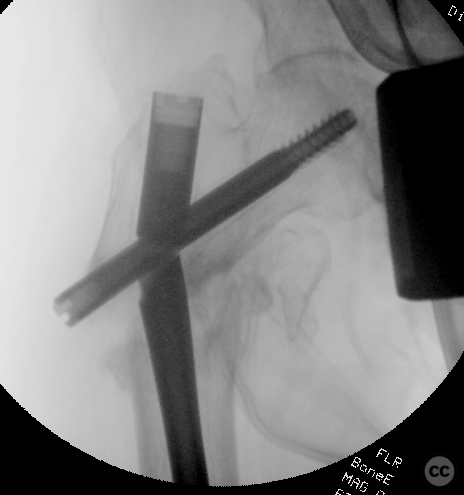
Operative remarks:The surgical approach was conducted on a traction table using a direct lateral approach, which facilitated the removal of the existing hardware, including the broken gamma nail. This was accomplished using the double wire back slap technique, where both a ball tip and a smooth guide wire were introduced, exiting through the distal aspect of the nail. Retraction of the ball tip guide wire allowed for wedging and subsequent backslapping of the nail in a retrograde manner, leading to its complete removal. Following the removal of the hardware, oscillating saw resection of the non-union site was performed, along with a planned valgus osteotomy. The initial saw cut osteotomy was secured using a single lag screw across the osteotomy site. Subsequently, a Synthes stainless steel proximal femoral locking plate was applied, utilizing 7.3 mm locked screws in the proximal aspect of the plate. The plate was fitted in a proximal-fragment-first manner (akin to the 'distal-fragment-first' technique used in distal radius fractures). The locked angle proximal screws were inserted and fixed into the plate, while the distal aspect of the plate was elevated slightly from the distal femoral diaphysis. This positioning allowed for effective reduction of the plate to the diaphysis resulting in dynamic valgization of the proximal neck by an additional five degrees. The surgical outcome yielded an good final valgus inclination of the proximal fragment, with optimal dynamic compression over the plate at the osteotomy site. This site was also augmented with morselized bone fragments obtained during the pseudoarthrosis resection. Samples were taken for microbiological analysis to confirm the absence of infection; however, there was no clinical suspicion of infection at the time.
Postoperative protocol: 50% Weightbearing
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities









User Discussion (1)
Guest User
Good job
thanks :)