Peripheral posterior wall acetabular fracture dislocation
Score and Comment on this Case
Clinical Details
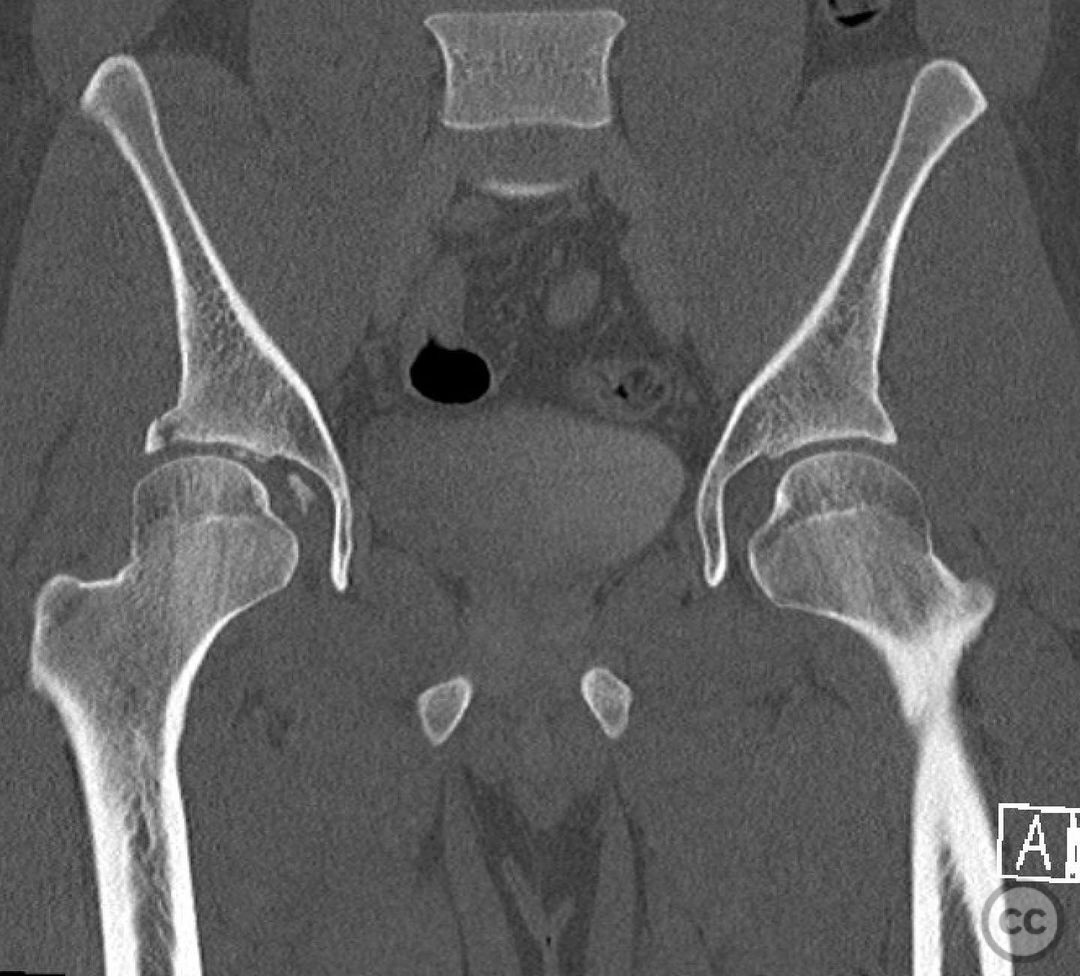
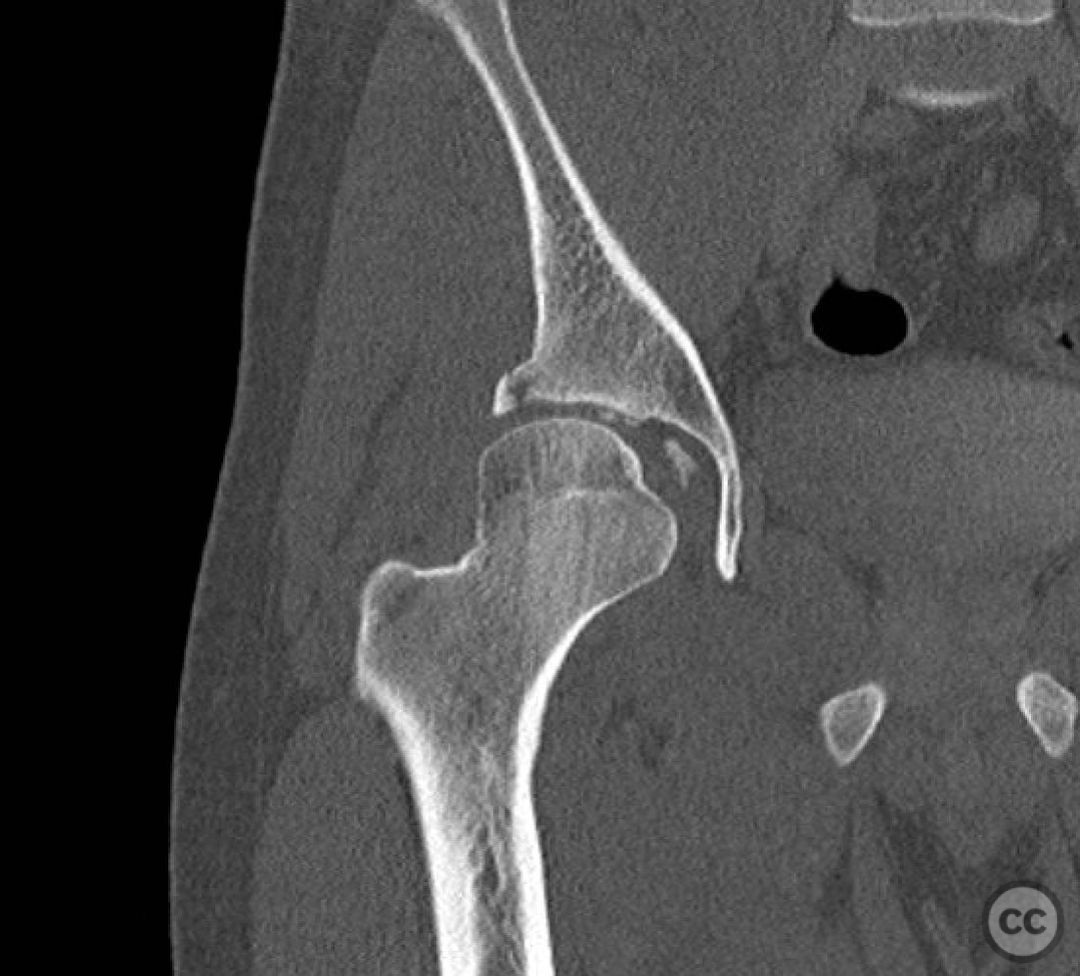
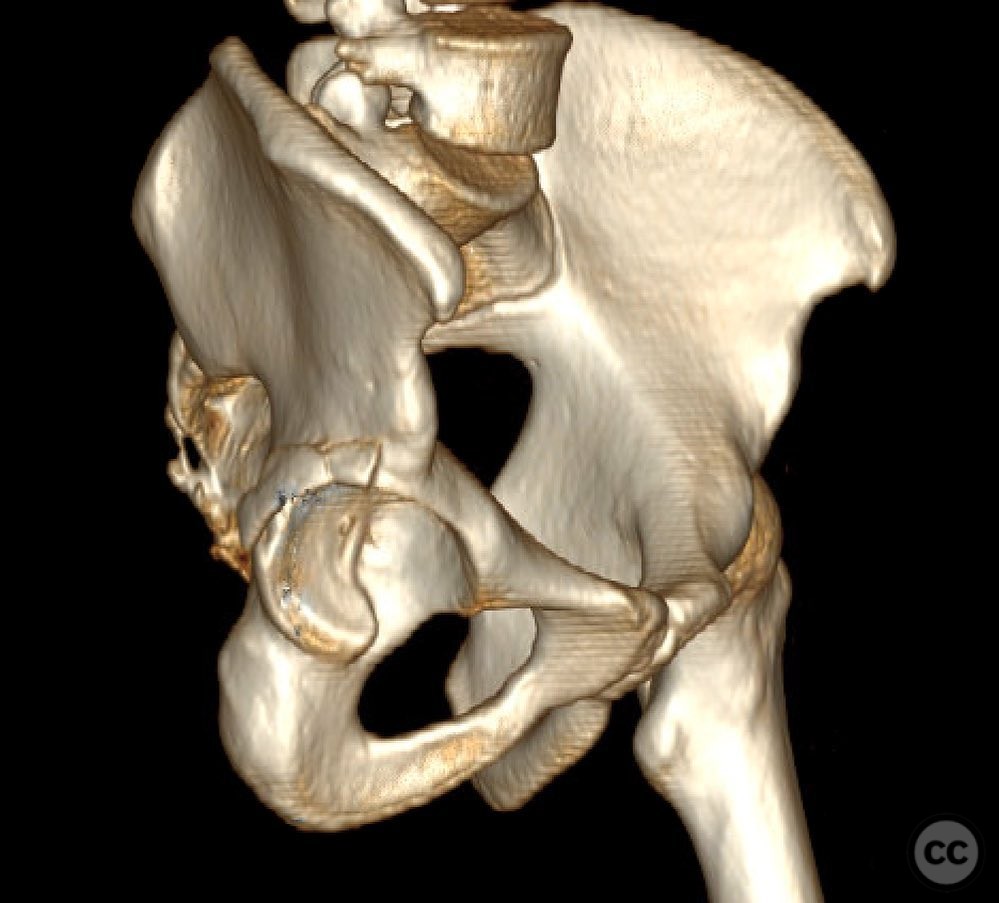
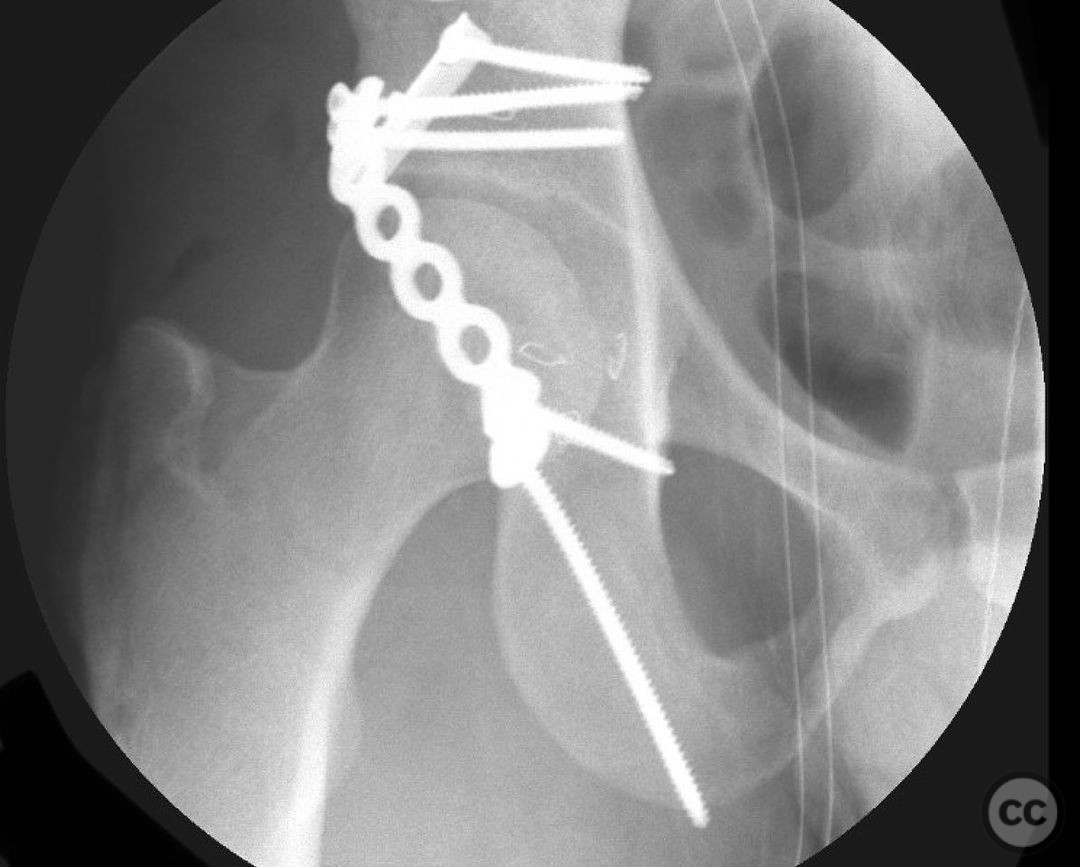
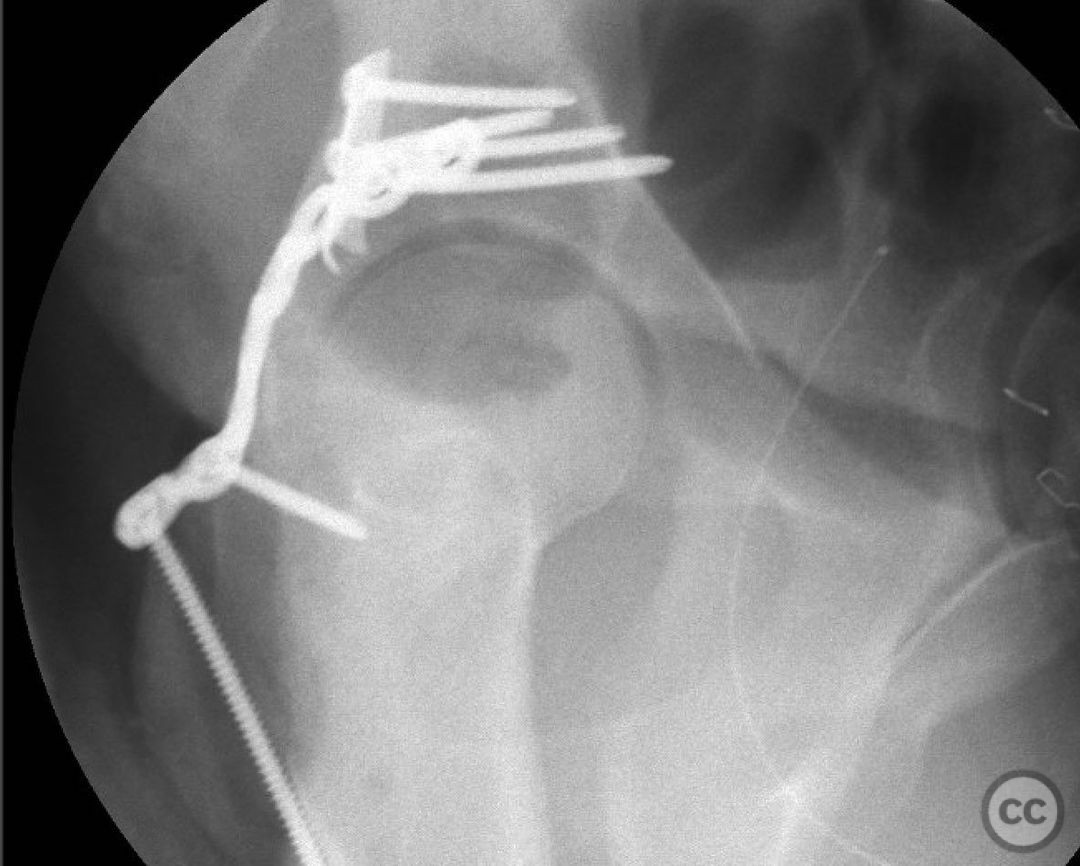
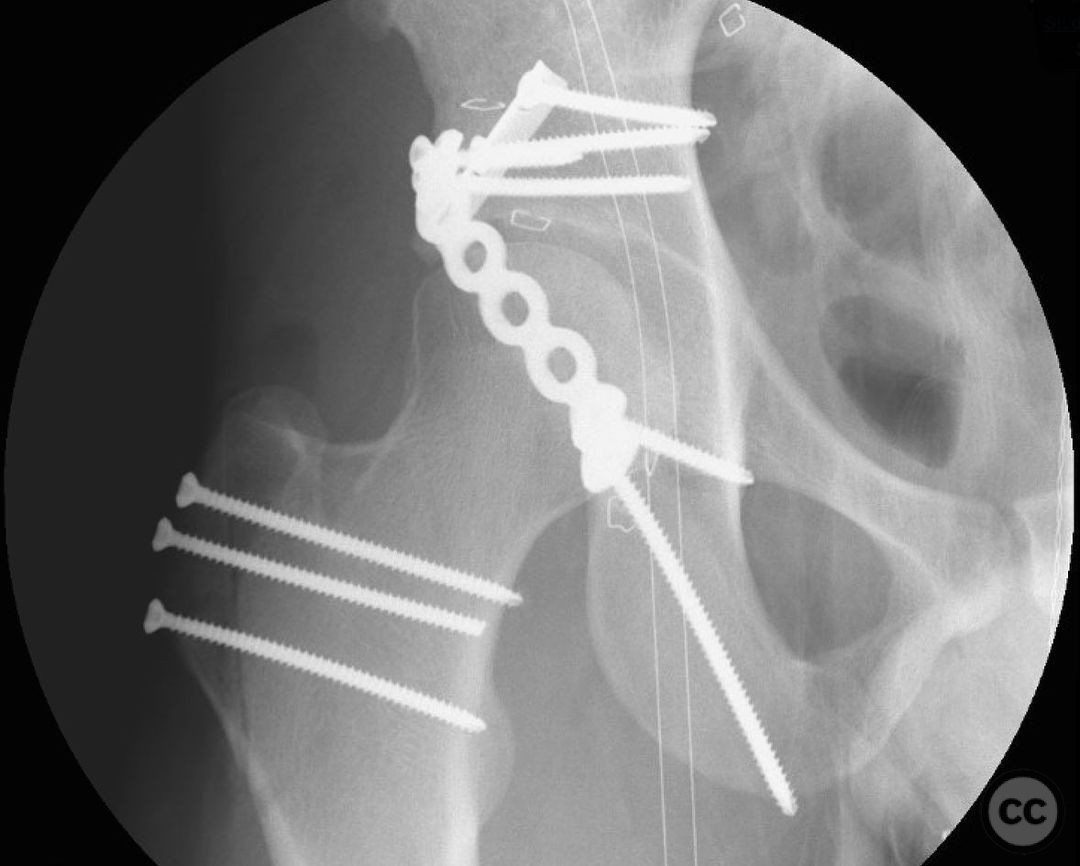
Clinical and radiological findings: This is a 22yo who sustained this very cranial (with anterior extension) peripheral posterior wall fracture dislocation. Other features important to identify- slightly dysplasic hip (likely contributing to the peripheral/cranial nature of this pattern, also plays into the discussion of post traumatic arthritis/arthroplasty), cranial marginal impaction, and free osteochondral fragments in the joint. All these things influence the treatment plan.
Preoperative Plan
Planning remarks:
Surgical Discussion
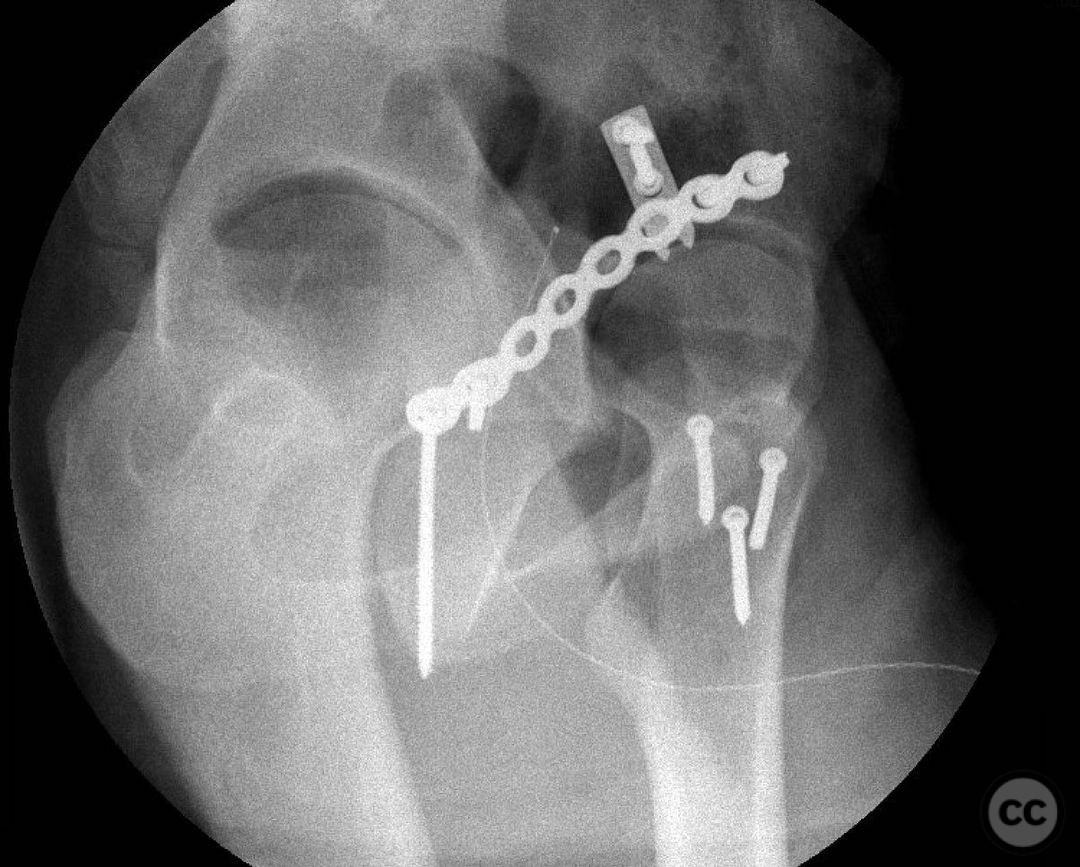
Operative remarks:For a pattern that extends well anterior midline, a trochanteric slide osteotomy provides improved anterior Supra-acetabular visualization and decreases trauma to the gluteus medius and superior gluteal neuro vascular bundle. A Gibson approach with the patient in the lateral position, combined with this osteotomy provides ideal access for this uncommon variant. If attempting to reduce and fix this through a standard KL, retraction on the medius and SGA/SGN is going to be problematic. Once the osteotomy is done, a distractor and a satinsky clamp are used to draw out intra-articular fragments and the caudal capsulolabral complex. Next task is to address marginal impaction to restore articular congruity- in this case you can see quite clearly on the fluro video that I initially missed a portion of the impaction, resulting in a big articular step-off. The plate was removed, the additional impacted are was identified, disimpacted, back filled and then fixed. The capsulolabral complex is repaired with soft tissue anchors caudally and a buttress plate is applied over the spring plate to reinforce fixation. In regards to the osteotomy, I will place a row of k-wires in the plane and in the planned location of the cut prior to making it to ensure the fragment isn’t too large or small. I like to pre-drill it for ease of repair at the end of a long case. Some surgeons will use a step cut but as Ganz points out, loss of reduction is unlikely due to the balanced pull between medius and vastus lateralis. In regards to primary THA in the setting of dysplasia, I think there is room for discussion
Author's Resources & References
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities



Article viewed 1057 times
15 Jan 2023
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2023). Peripheral posterior wall acetabular fracture dislocation. Journal of Orthopaedic Surgery and Traumatology. Case Report 39097636 Published Online Jan 15 2023.