Dynamic Hip Screw - Evans 2 Stable Intertrochanteric Fracture
Score and Comment on this Case
Clinical Details
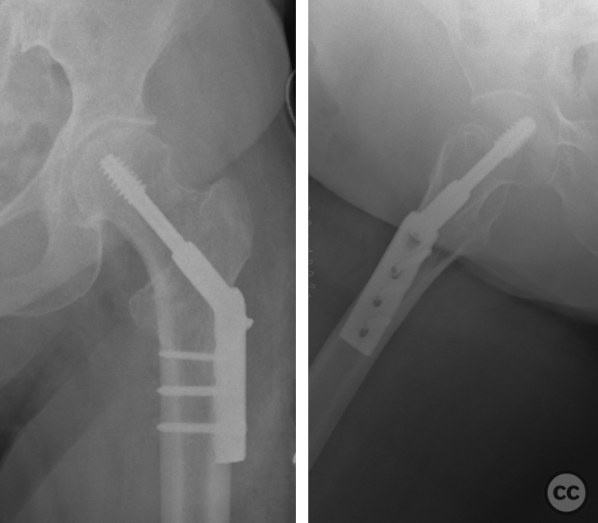
Clinical and radiological findings: A 68-year-old female patient presented to the emergency department after experiencing a simple fall, resulting in significant hip pain. Clinical examination revealed localized tenderness over the hip region, with restricted range of motion due to pain. Radiographic evaluation confirmed an intertrochanteric fracture, classified as an Evans 2 stable type, without evidence of additional pelvic or lower extremity fractures.
Preoperative Plan
Planning remarks: The preoperative plan included the application of a dynamic hip screw (DHS) system for dynamic fixation of the intertrochanteric fracture. The surgical approach was to be a limited transvastus approach.
Surgical Discussion
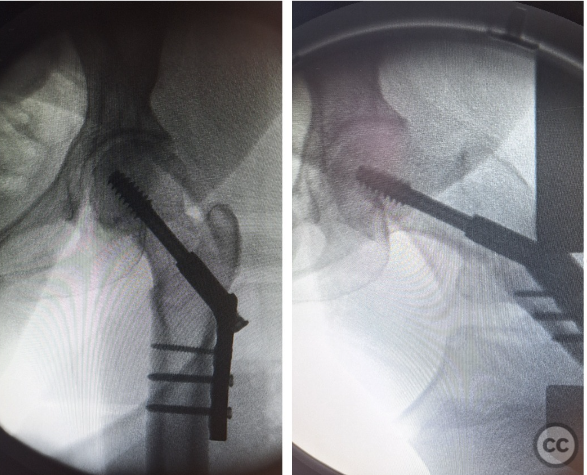
Patient positioning: The patient was positioned supine on a radiolucent operating table, with the affected leg prepared and draped in a sterile fashion. A traction table was not utilized; instead, manual traction and internal rotation were applied as needed to achieve fractur
Anatomical surgical approach: A lateral approach to the hip was employed, beginning with a longitudinal incision centered over the lesser trochanter. Subcutaneous tissues were dissected, and the fascia lata was incised in line with the skin incision. The vastus lateralis muscle was split and retracted anteriorly to expose the lateral aspect of the femur.
Operative remarks:Intraoperatively, after achieving satisfactory fracture reduction under fluoroscopic guidance, the dynamic hip screw was positioned on the lateral cortex of the femur. A guide wire for the DHS was inserted into the femoral head, aiming for center-center/inferior placement in both anteroposterior and lateral views. The DHS plate was then affixed to the femoral shaft with cortical screws. Intraoperative imaging confirmed appropriate placement of hardware and satisfactory fracture alignment.
Postoperative protocol: Postoperative rehabilitation protocol included early mobilization with weight-bearing as tolerated, guided by pain levels and stability of the surgical fixation. Physical therapy focused on restoring range of motion, strength, and gait training commenced on the first postoperative day.
Follow up: Not specified
Orthopaedic implants used: Dynamic hip screw (DHS) system.
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisA total of 12 articles were analysed in the generation of this review, of which 10 were considered relevant for inclusion. The types of articles included randomized clinical trials, retrospective comparative studies, register-based studies, and descriptive epidemiological register studies. The evidence level ranged from high-quality randomized controlled trials to large national registry analyses and retrospective observational studies. The publication dates span from 2011 to 2023.
Evidence: The comparison between dynamic hip screw (DHS) and intramedullary nail (IMN) fixation for intertrochanteric femur fractures has been a subject of extensive investigation due to the prevalence and impact of these injuries [1-10]. Studies have explored various outcomes including mortality rates, functional outcomes, complication rates including reoperation rates, operative time, blood loss during surgery, radiation exposure during surgery (DAP), length of hospital stay post-surgery, and cost-effectiveness.
The INSITE Randomized Clinical Trial found no significant differences in health-related quality-of-life scores at one year post-surgery between patients treated with IMNs versus those treated with DHSs [3]. This study suggests that both treatment options provide comparable outcomes in terms of patient quality of life following surgery. However, it is noted that IMNs may offer some advantages in specific fracture patterns or patient populations.
A study from the Norwegian Hip Fracture Register indicated lower reoperation rates for unstable trochanteric and subtrochanteric fractures when treated with IMN compared to DHS but found no difference for stable fractures [6]. This suggests that fracture stability might play a crucial role in deciding the optimal fixation method.
Comparative analysis on peri-operative outcome measures showed significantly lower mean blood loss and radiation DAP for DHS compared to IMN group [4], suggesting potential benefits regarding intraoperative safety parameters when using DHS. Conversely, another study highlighted increased operative time but decreased fluoroscopy X-ray exposure time with DHS fixation compared to EBA nailing [9].
Regarding morbidity and mortality analysis comparing DHS vs TFNA (a type of intramedullary nail), one study concluded that TFNA demonstrated superior results concerning full weight-bearing at hospital discharge especially for treating unstable trochanteric hip fractures [5]. However, it was also noted that longer times from diagnosis to surgery were associated with increased mortality across both groups indicating the importance of timely surgical intervention regardless of chosen fixation method.
Therapy Synopsis:
Considering the evidence synthesized from available literature comparing dynamic hip screw (DHS) versus intramedullary nail (IMN) fixation methods for intertrochanteric femur fractures; while both methods show similar outcomes in terms health-related quality-of-life scores at one year post-surgery as well as other key metrics such as mortality rates - there are nuanced differences which can guide clinical decision-making based on specific circumstances such as fracture stability where IMNs may offer an advantage over DHSs particularly for unstable trochanteric or subtrochanteric fractures due their lower reoperation rate as per findings from large registry data. Additionally considering intraoperative factors like reduced blood loss favoring DHS could be relevant under certain clinical scenarios necessitating minimization of surgical risk factors. Given these considerations alongside economic implications where applicable; our recommendation leans towards utilizing Intramedullary Nails primarily for unstable trochanteric/subtrochanteric femur fractures given their slight edge in reducing reoperations whilst acknowledging Dynamic Hip Screws' value under conditions warranting its selection based on individual patient needs or surgeon preference taking into account all aforementioned factors comprehensively.
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities


User Discussion (1)
Guest User
May be better with an additional antirotation cannulated screw