Progressive Scoliosis Correction via Pan Genu Epiphysiodesis with Tension Band Plates
Score and Comment on this Case
Clinical Details
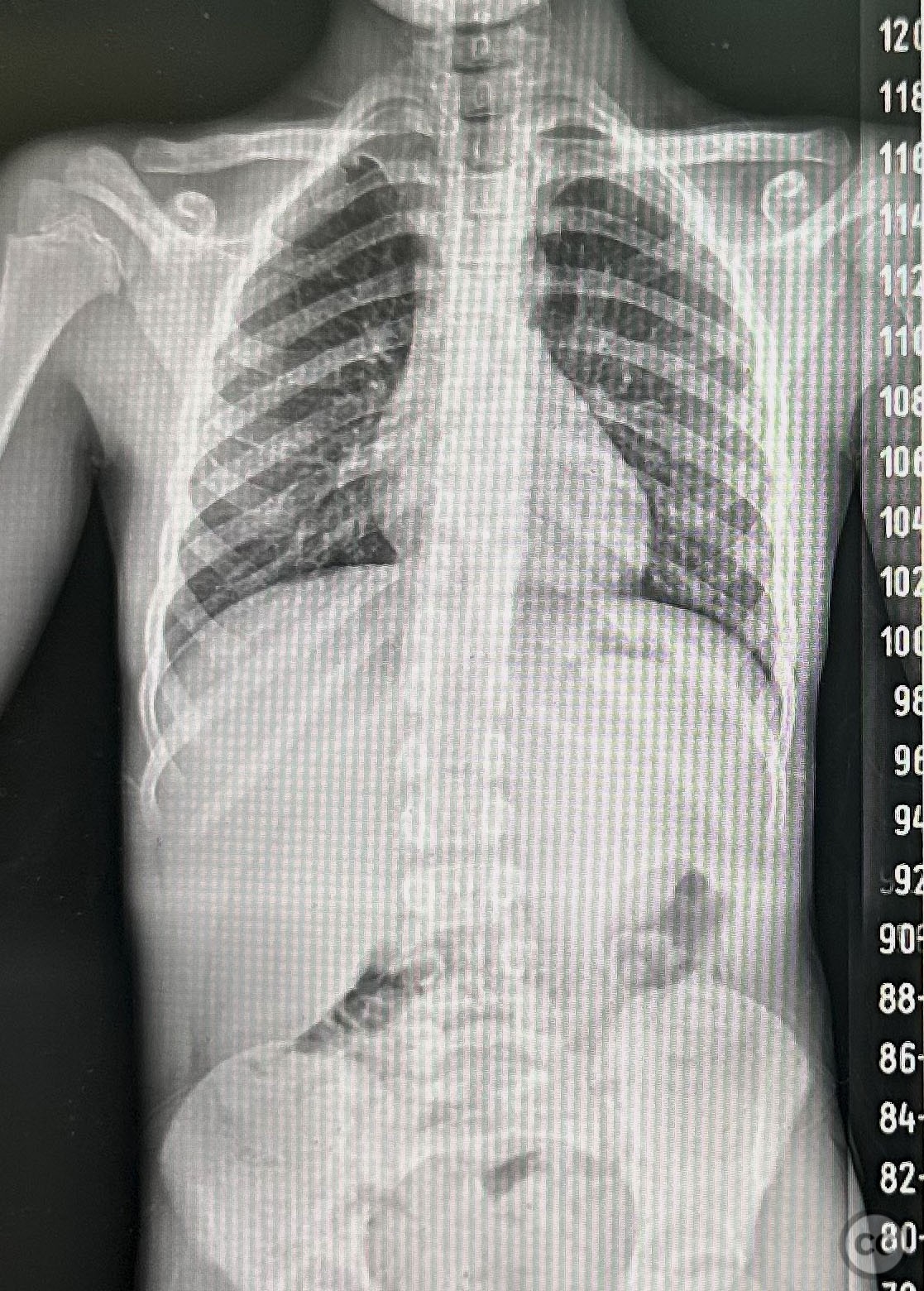
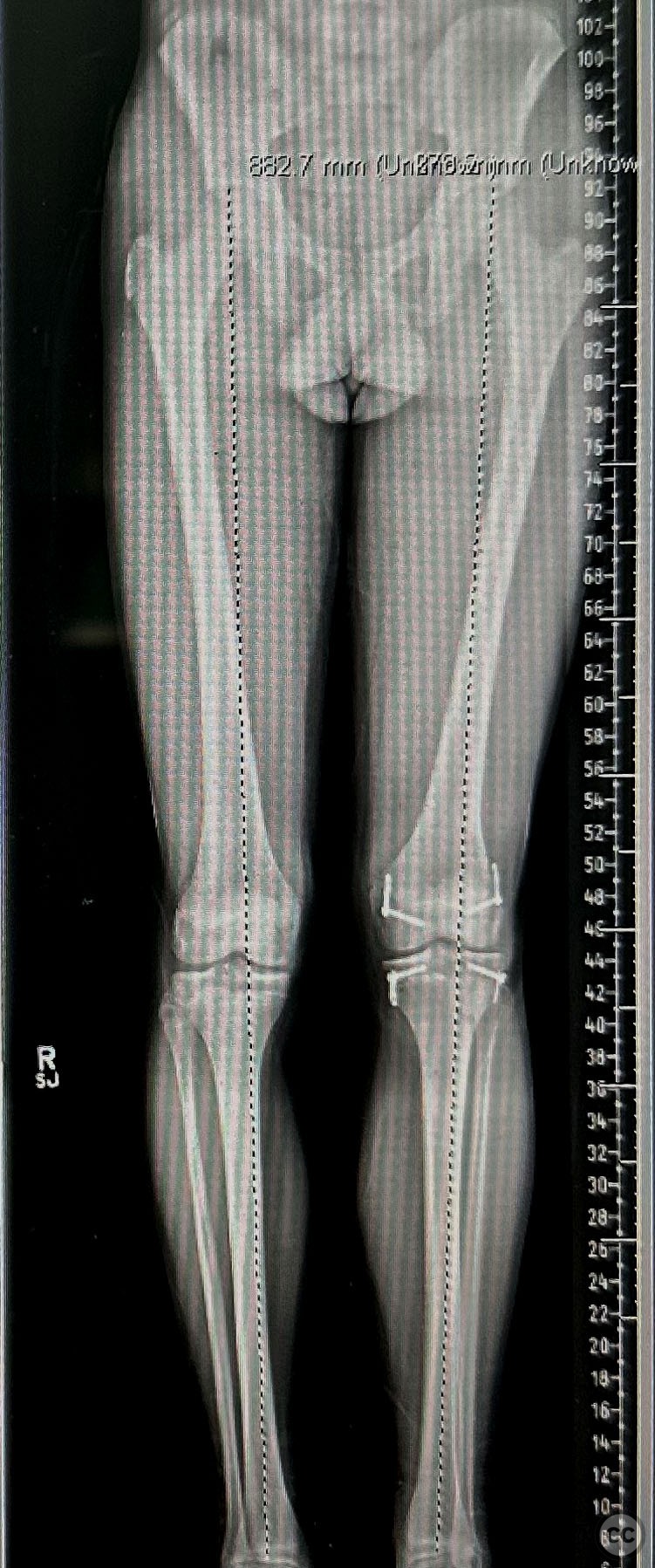
Clinical and radiological findings: Patient presented with progressive scoliosis exceeding 25 degrees, accompanied by a noticeable leg length discrepancy (LLD). The condition was identified during routine clinical evaluation, with radiographic imaging confirming the scoliosis and LLD without additional vertebral anomalies or systemic conditions.
Preoperative Plan
Planning remarks: The preoperative plan included unilateral pan-genu epiphysiodesis utilizing tension band plates to address the LLD and indirectly influence the scoliosis curvature. The approach aimed at halting the growth on the longer leg's distal femur and proximal tibia to allow the shorter leg to catch up, thereby reducing LLD and scoliosis.
Surgical Discussion
Patient positioning: Supine position
Anatomical surgical approach: Anteromedial and anterolateral approaches to the knee were employed. Incisions were made over the distal femur and proximal tibia to expose the growth plates. Tension band plates were positioned across the growth plates of both the distal femur and proximal tibia, ensuring accurate alignment to effectively modulate growth.
Operative remarks:Intraoperatively, attention was given to the symmetrical placement of tension band plates across the growth plates to ensure balanced growth arrest. The procedure aimed at correcting the LLD, thereby indirectly influencing the reduction of scoliosis curvature. Postoperative imaging confirmed the placement of tension band plates.
Postoperative protocol: Postoperative rehabilitation focused on early mobilization with weight-bearing as tolerated, guided by pain levels and stability. Range of motion exercises were initiated immediately post-surgery.
Follow up: Not specified.
Orthopaedic implants used: Tension band plates and screws designed for growth modulation. No specifics provided.
Search for Related Literature
Industry Sponsership
contact us for advertising opportunities




Article viewed 348 times
12 Mar 2024
Add to Bookmarks
Full Citation
Cite this article:
David Bennett. (2024). Progressive Scoliosis Correction via Pan Genu Epiphysiodesis with Tension Band Plates. Journal of Orthopaedic Surgery and Traumatology. Case Report 40610601 Published Online Mar 12 2024.