Percutaneous Cannulated Screw Fixation of a Triplanar Distal Tibial Physeal Fracture
Score and Comment on this Case
Clinical Details
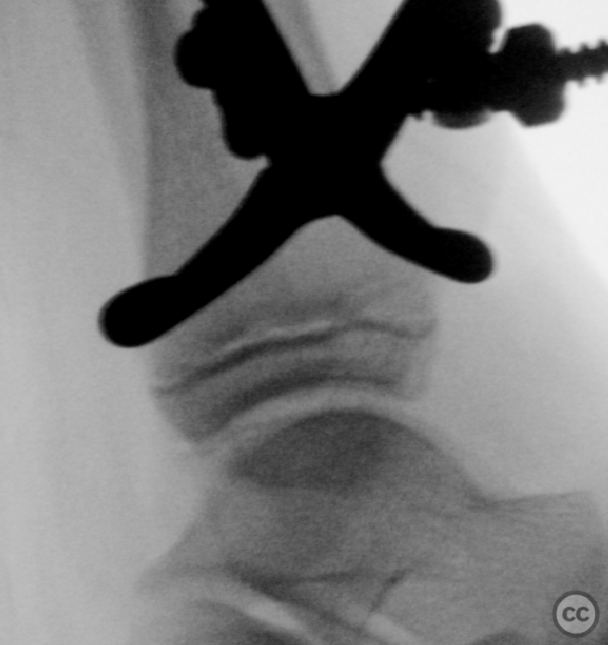
Clinical and radiological findings: A 9-year-old male presented with pain and swelling to the right ankle and an inability to bear weight following a fall in the schoolyard. Plain radiographs revealed a triplanar distal tibial physeal fracture. Subsequent CT imaging confirmed the diagnosis and provided detailed 3D visualization for operative planning.
Preoperative Plan
Planning remarks: The preoperative plan included closed reduction and percutaneous physis-sparing screw fixation of the fracture, with screws placed proximal and distal to the physis to avoid physeal damage.
Surgical Discussion
Patient positioning: The patient was positioned supine on the operating table.
Anatomical surgical approach: After unsuccessful closed reduction under simple manipulation, a stab incision was made posterior to the fibula for the insertion of a pointed reduction clamp. Anteroposterior clamping of the metaphyseal fracture fragment was performed under further closed manipulation until a spontaneous, sudden anatomic reduction was achieved with an audible 'click'.
Operative remarks:Under fluoroscopic guidance, two 4.0mm cannulated screws were inserted anteroposteriorly across the fracture site, avoiding the physis. An additional anteromedial 4.0mm cannulated screw was placed based on preoperative CT scan trajectory planning to ensure optimal fixation.
Postoperative protocol: Postoperatively, the patient's ankle was immobilized in an orthosis with instructions for 6 weeks of partial weight bearing. The hardware was scheduled for removal between 3 to 6 months postoperatively.
Orthopaedic implants used: Two 4.0mm cannulated screws (anteroposterior placement) - One 4.0mm cannulated screw (anteromedial placement)
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisPaediatric triplane physeal tibial fractures represent a unique injury pattern that occurs during the transitional phase of skeletal maturation when the distal tibial physis closes asymmetrically [1]. These injuries typically occur between ages 10 to 15 due to an external rotation mechanism on the ankle, leading to fracture lines propagating through three planes: axial, sagittal, and coronal [5, 7, 8].
Recent literature has however challenged traditional teachings regarding these injuries. A study utilizing fracture mapping techniques revealed that regardless of age or sex, triplane ankle fractures consolidate into a characteristic Y-pattern without shifting with physeal closure. This suggests that ligament attachments play a significant role in influencing fracture patterns rather than just physeal closure alone.
Given the complexity of these fractures and their potential to impact long-term growth, accurate classification and appropriate treatment planning are critical. The utilization of computed tomography (CT) has been shown to significantly impact fracture classification, displacement measurement, and treatment planning, suggesting its importance as an adjunctive tool to radiographs [5]. This is supported by evidence demonstrating improved accuracy in diagnosing triplane fractures with CT, especially among more experienced surgeons [6].
Furthermore, a new classification system based on axial CT scans has been proposed, which could optimize screw trajectory during surgical intervention [9]. In the treatment of triplane fractures, both non-operative (closed reduction and casting) and operative (open reduction and internal fixation) strategies have been employed. The decision between these approaches is often determined by the degree of displacement and fracture instability [11, 12, 14].
Studies have shown that non-operative treatment can yield satisfactory outcomes for fractures with minimal displacement [12, 13]. However, for fractures with displacement greater than 2 mm, surgical intervention is typically indicated to minimize the risk of long-term complications, such as degenerative joint disease and growth disturbances [10, 11, 14]. Comparative studies have evaluated different fixation techniques, such as lag screw versus Kirschner wire fixation, with the former showing a lower rate of premature physeal closure [3]. Moreover, case reports and retrospective case series have highlighted the importance of considering atypical triplane fracture patterns and the role of percutaneous screw fixation in achieving anatomic reduction and earlier mobilization [4, 7].
Despite the evidence provided, the literature also reveals the possibility of missed or delayed diagnosis, particularly in the presence of concurrent ipsilateral tibial shaft fractures [2, 11]. This underscores the need for a high index of suspicion and thorough clinical and radiographic assessment to prevent overlooking these significant injuries.
In summary, the current evidence indicates that while non-operative treatment may be adequate for non-displaced or minimally displaced triplane fractures, displaced fractures generally require operative intervention to restore anatomic alignment and prevent growth disturbances and degenerative changes. The application of CT scans has improved the classification and treatment planning for these fractures, thereby influencing outcomes positively.
Author's Resources & References
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities










Article viewed 1816 times
09 Feb 2024
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2024). Percutaneous Cannulated Screw Fixation of a Triplanar Distal Tibial Physeal Fracture. Journal of Orthopaedic Surgery and Traumatology. Case Report 41609863 Published Online Feb 09 2024.