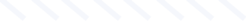
Complex comminuted and impacted distal radius fracture
Score and Comment on this Case
Clinical Details
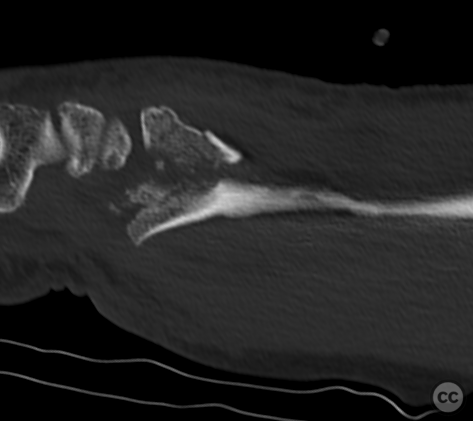
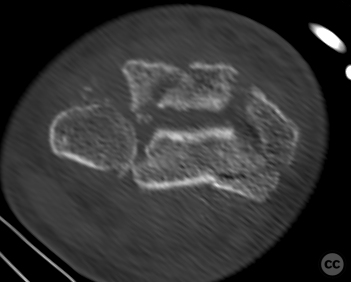
Clinical and radiological findings: A 62-year-old male farmer presented with a closed, neurovascularly intact injury to the right distal radius following a fall from the roof of a shed. Plain film and CT imaging revealed a multifragmentary, impacted, dorsally displaced fracture of the distal radius. The articular surface was split with fragmentation and impaction of the scaphoid and lunate fossae, including a marked central depression of a volar lunate fossa fragment.
Preoperative Plan
Planning remarks: The preoperative plan included open reduction and internal fixation with the goal of anatomically reconstructing the articular surface, restoring radial length, inclination, and volar tilt, and addressing any carpal subluxation. A volar approach was chosen to directly visualize and manipulate the volar lunate fossa fragment and other volarly displaced fragments, and secure the volar rim.
Surgical Discussion
Patient positioning: The patient was positioned supine on a radiolucent operating table
Anatomical surgical approach: A volar Henry approach was utilized, starting with an approximately 8 cm longitudinal incision over the flexor carpi radialis (FCR) tendon, extending in a zigzag fashion across the distal wrist crease. Subcutaneous dissection was followed by incision of the FCR sheath and release of distal connective tissue (Mercer) fibers. The fascia overlying the flexor pollicis longus (FPL) was incised, and the FPL tendon was retracted ulnarly. A radial incision along the border of pronator quadratus was made, and the muscle was elevated with a periosteal elevator to expose the fracture.
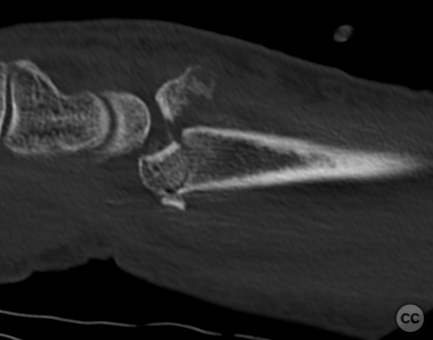
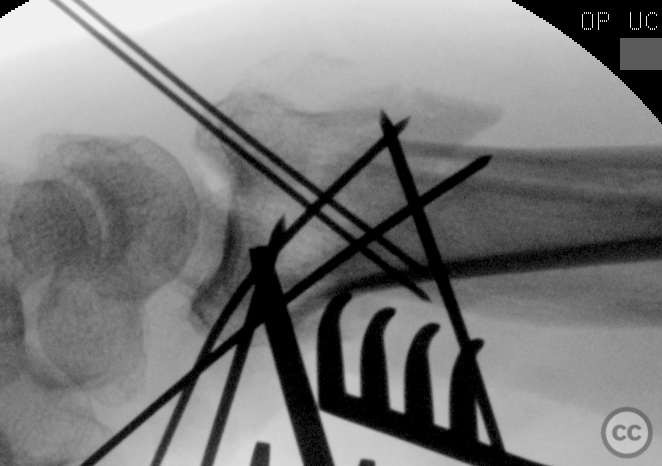
Operative remarks:Intraoperatively, the volar lunate fossa fragment was elevated with abn osteotome and provisionally pinned with 1.0 mm K-wires from the articular rim. Dorsal fragments were percutaneously secured with K-wires and reduced to the volar fragments using joystick technique. The radial styloid fragment was mobilized and anatomically reduced under fluoroscopic guidance utilising a Hintermann K-Wire retractor.
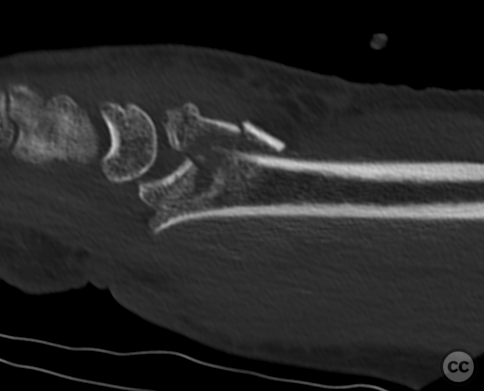
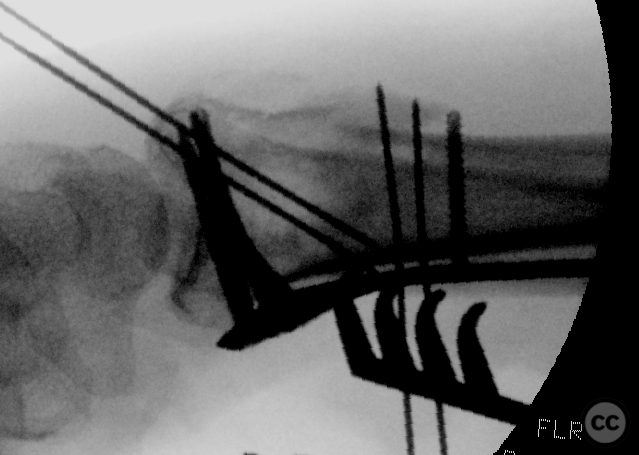
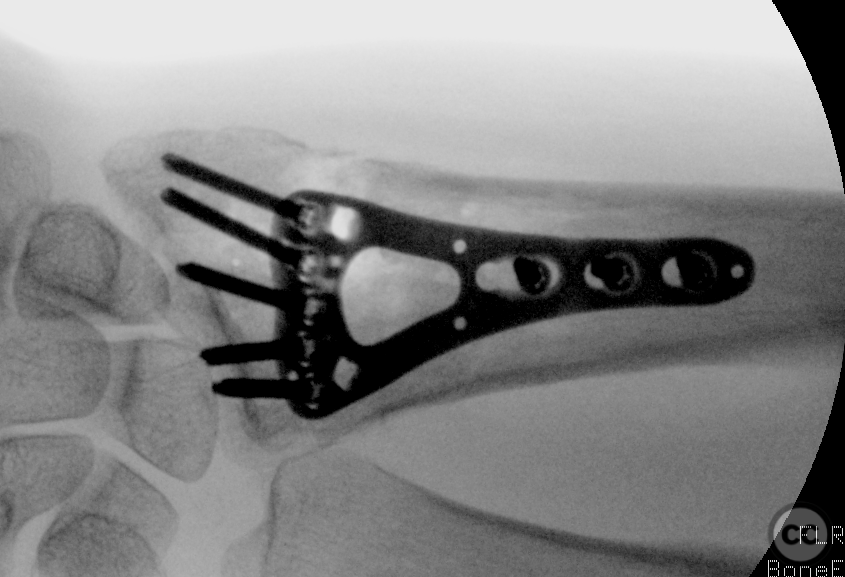
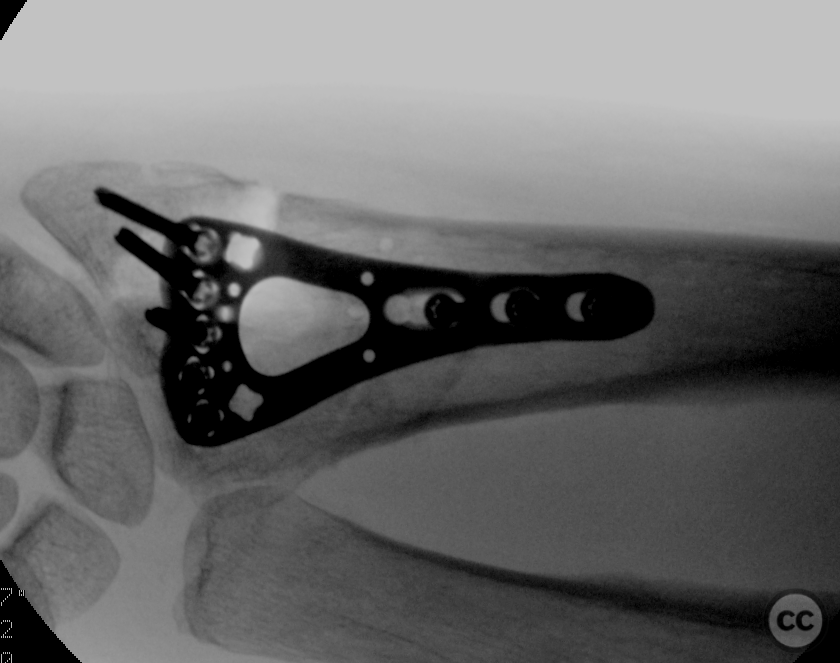
A two-column volar plate was positioned using a distal-first technique, securing the fragments with subchondral screws. The plate was then dynamically reduced to the radial shaft, allowing fine manipulation of fracture alignment and restoration of radial length, inclination, and volar tilt. Final fixation was achieved with bicortical screws.
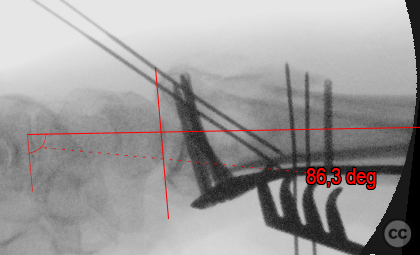
The final lateral fluroscopy image failed to really hit the joint axis. Previous shots demonstrated good reduction. When the joint proves hard to align on fluro, it usually means somethings not quite right in the reduction, but given the complexity of this case, and the encouraging previous images, no revision was attempted.
Postoperative protocol: Postoperative rehabilitation protocol included no immobilization, with full passive range of motion exercises initiated immediately under non-weight-bearing conditions for six weeks.
Follow up: Not specified.
Orthopaedic implants used: Multiple K-wires, Synthes two-column volar DRP.
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisThe management strategy for central die-punch injuries primarily revolves around restoring the congruity of the articular surface and maintaining stable fixation to allow for early mobilization. Surgical treatment options include open reduction internal fixation (ORIF) using volar locking plates (VLP), external fixation, or a combination thereof [1,2].
Lee et al.'s study highlights that articular surface mismatch significantly affects surgical outcomes when treating distal radius fractures with VLPs. Specifically, mismatches in the dorsal lunate facet and central depression have been correlated with worse Disabilities of Arm Shoulder and Hand (DASH) scores and Modified Mayo Wrist Scores (MMWS). This underscores the importance of meticulous reduction efforts in these areas [1]. Furthermore, Lee et al.'s findings suggest that particular attention should be paid to reducing dorsal lunate facet involvement as it is a significant predictor for poorer MMWS outcomes.
Porter and Tillman's work provides insight into pilon fractures involving high-energy wrist injuries leading to complex articular disruptions including central die-punch lesions. Their study emphasizes that while external fixators may maintain extra-articular alignment effectively, they fall short in ensuring accurate articular surface reduction. Residual joint incongruity was identified as an adverse prognostic feature; patients with more than 2mm step-off on the joint line developed symptomatic arthritis at higher rates [2].
Both pieces highlight critical aspects in managing central die-punch injuries - achieving anatomical restoration of the joint surface is paramount. Given these insights, current best practices would involve using advanced imaging techniques like CT scans preoperatively for detailed fracture mapping followed by ORIF utilizing VLP or other suitable hardware tailored towards addressing specific fracture characteristics observed.
In cases where direct visualization or reduction through volar approaches proves challenging due to complex fracture patterns or dorsal fragment involvement, supplemental techniques such as arthroscopy-assisted reductions or dorsal plating might be warranted [1]. Additionally, considering Porter & Tillman's observations regarding associated ligamentous injuries' impact on outcomes [2], thorough evaluation for such concomitant damages during surgery is crucial; addressing them concurrently could potentially improve functional results.
In conclusion, effective management of central die-punch lesions within distal radius fractures requires a nuanced approach focused on precise anatomical restoration coupled with stable internal fixation strategies conducive to early rehabilitation efforts. Future research should aim at refining surgical techniques further and exploring novel fixation devices designed specifically for optimizing outcomes in these challenging injury patterns.
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant
Industry Sponsership
contact us for advertising opportunities











Article viewed 1270 times
21 Feb 2024
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2024). Complex comminuted and impacted distal radius fracture. Journal of Orthopaedic Surgery and Traumatology. Case Report 41827553 Published Online Feb 21 2024.