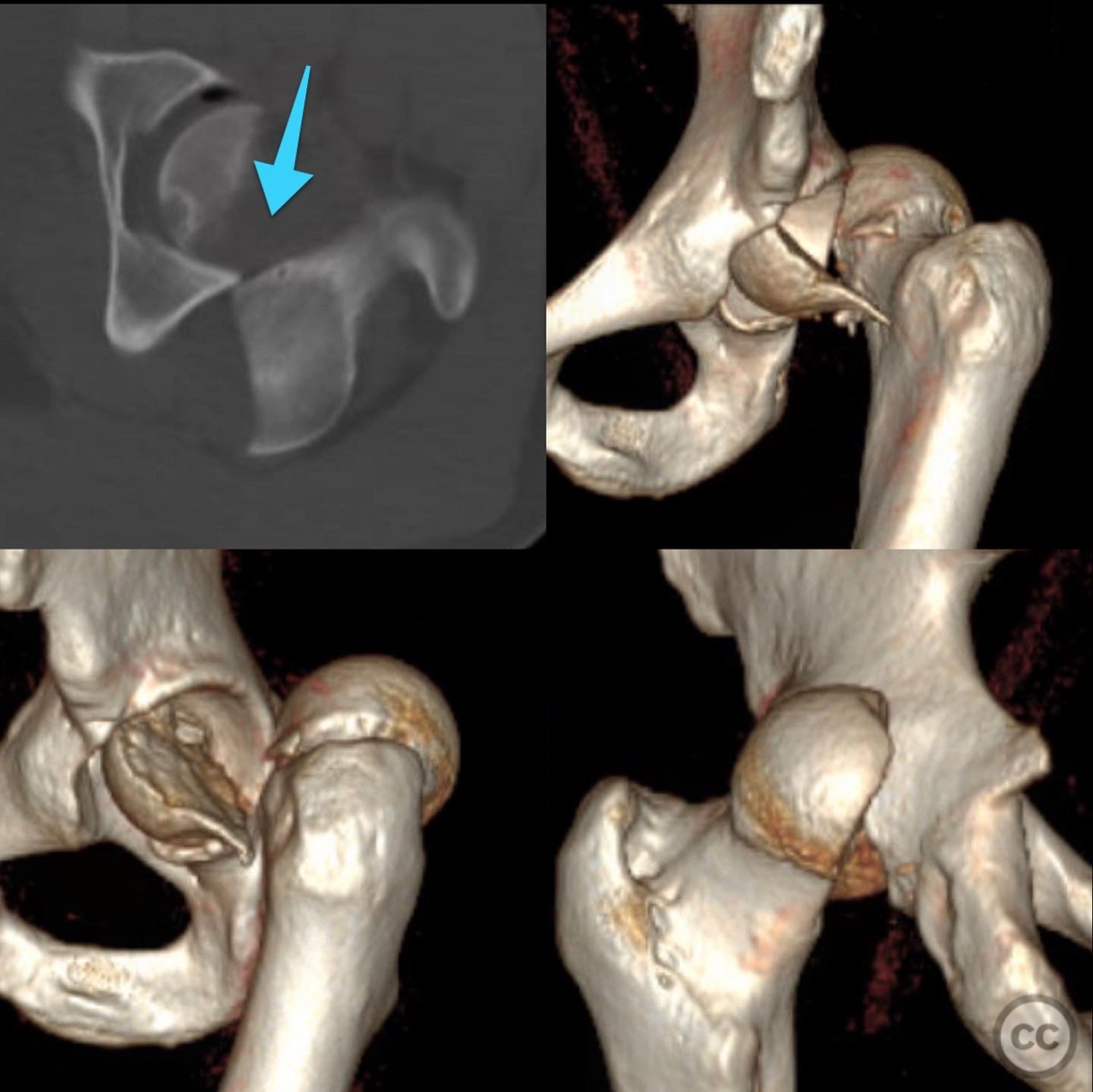
Femoral Head Fracture (Pipkin II) Treated with Surgical Dislocation / Trochanteric Osteotomy
Score and Comment on this Case
Clinical Details
Clinical and radiological findings: Patient is a young adult male involved in high-speed motor vehicle accident with isolated injury consisting of large femoral head fracture with irreducible posterior hip dislocation. No other medical comorbidities, hemodyanmically stable, neurovascular exam normal.
Preoperative Plan
Planning remarks: Plan
Surgical Discussion
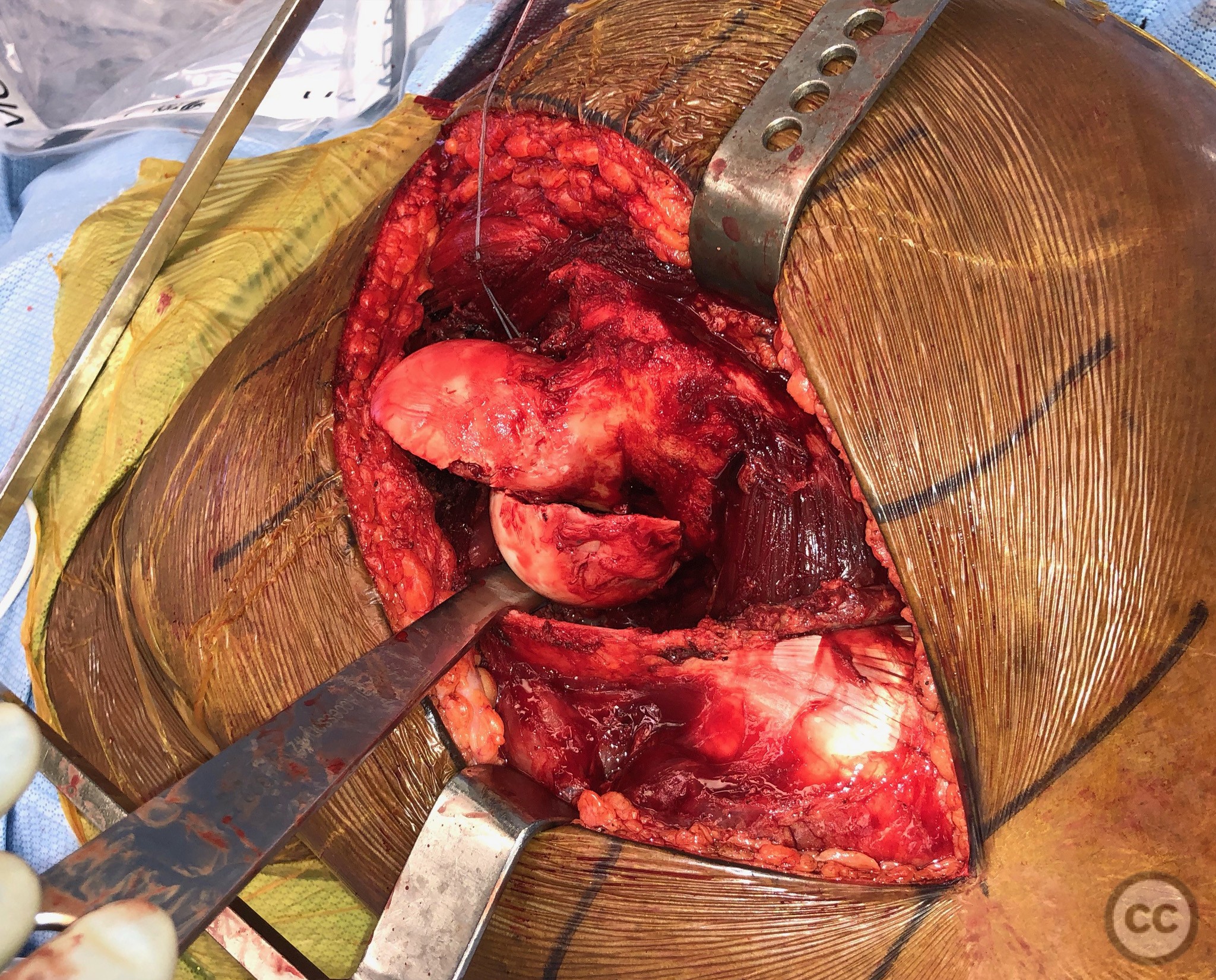
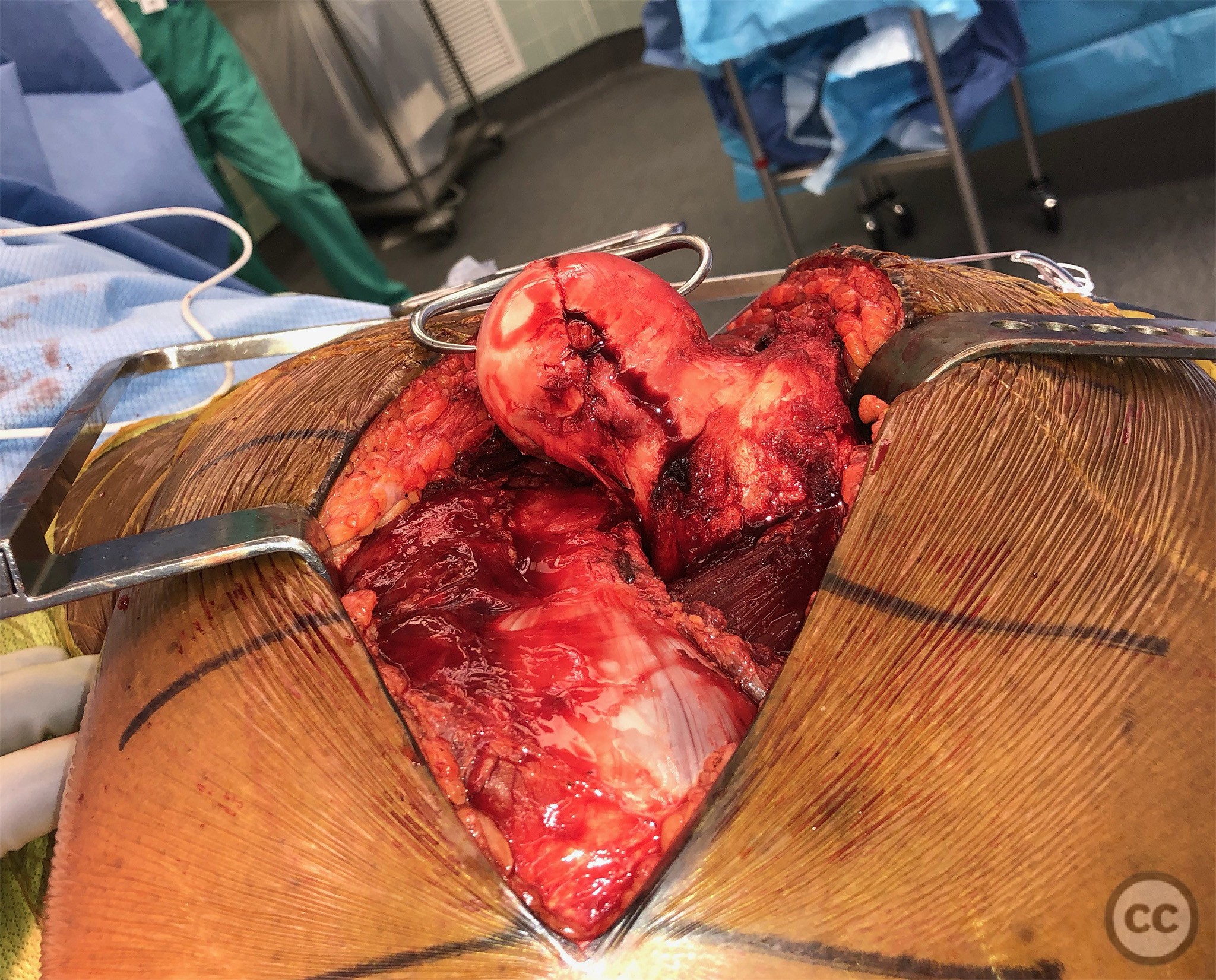
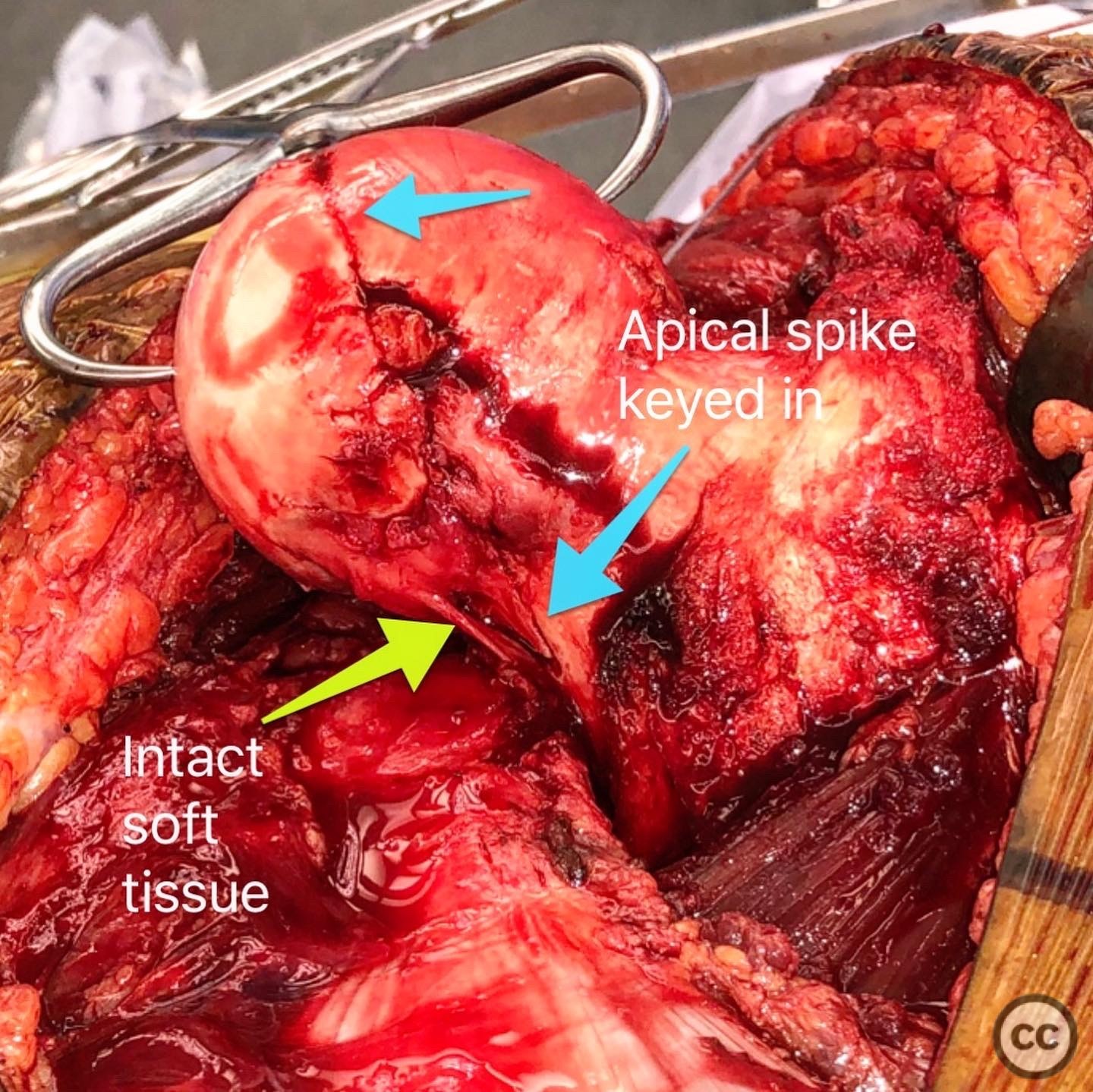
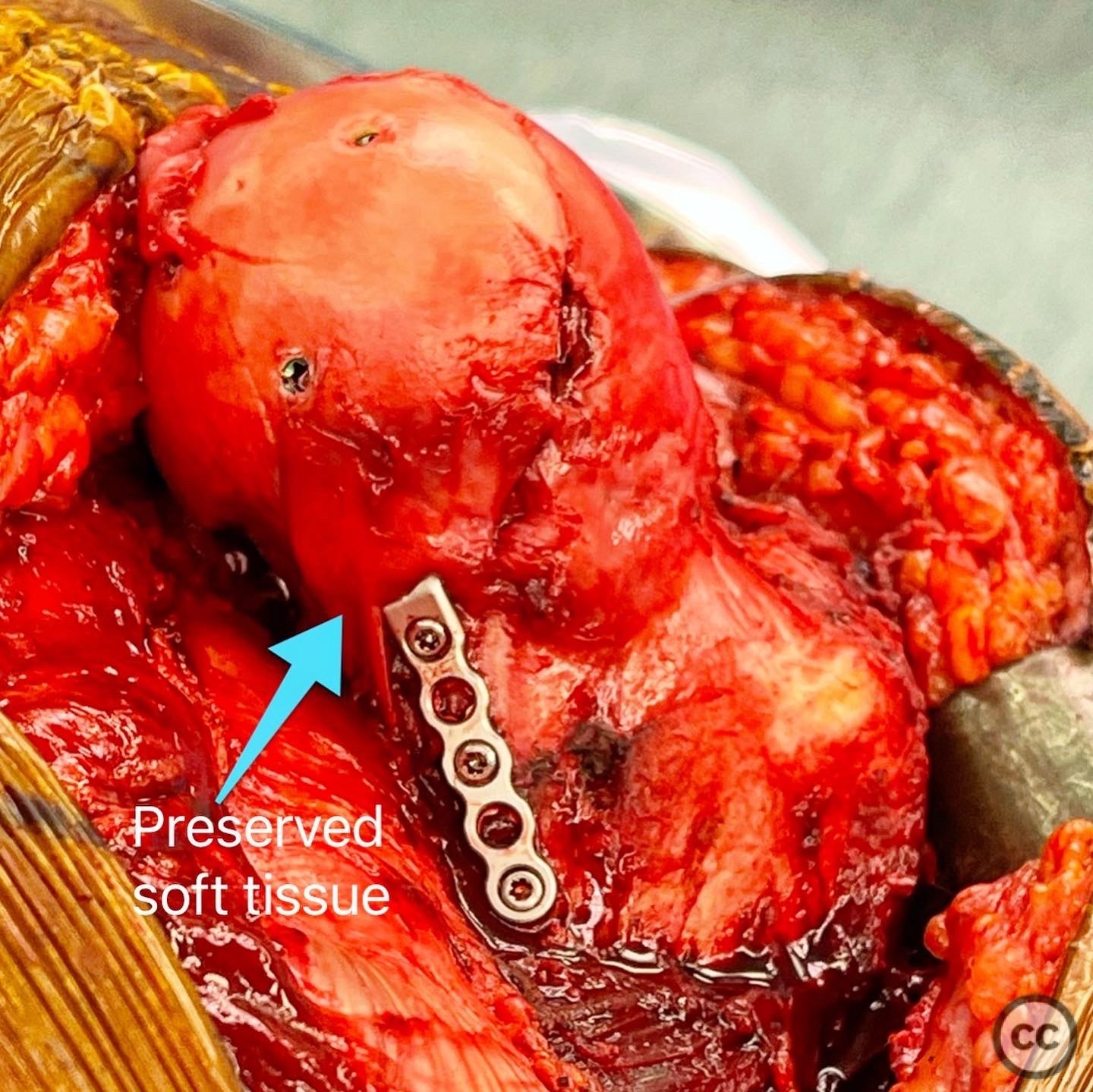
Operative remarks:Patient positioned lateral decubitus and digastric trochanteric osteotomy performed preserving abductor and vastus attachments. Fragment displaced anteriorly and surgical dislocation performed after anterior Z-capsulotomy. Displaced femoral head fragment identified and inferior capsular attachments preserved at femoral neck spike inferiorly. Fracture reduced with clamps and stabilized with headless compression screws. Because of neck extension, an antiglide minifrag plate was used to provide additional resistance to shear. Hip reduced and then trochanteric osteotomy stabilized with standard 3.5 cortical screws. Patient toe-touch weightbearing for 8 weeks with posterior hip precautions.
Orthopaedic implants used: Synthes 4.0 headless compression screws, Smith and Nephew EVOS mini fragment plate, Synthes 3.5 cortical screws
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisThe case report presented in [1] describes the management of a Pipkin II femoral head fracture utilizing surgical dislocation and trochanteric osteotomy. Pipkin fractures are rare, associated with hip dislocations, and have poor prognosis [4,5]. Surgical management of Pipkin type IV fractures is technically demanding, particularly in patients with high BMI [6]. In this context, a comprehensive literature review was conducted to assess the surgical technique and controversies surrounding the management of these fractures.
Surgical dislocation with trochanteric osteotomy has been used for various indications, including the treatment of femoral head osteochondral defects [19] and femoroacetabular impingement [20]. The modified lateral approach, a variant of surgical dislocation without trochanteric osteotomy, has been suggested as a safe, simpler, and effective alternative [20]. However, the comparison of outcomes between these approaches is limited in the literature.
Some studies have evaluated the Ganz approach for Pipkin fracture dislocations. A prospective, nonrandomized study involving 28 patients with type I/II Pipkin fractures reported low incidence of femoral head osteonecrosis and favorable clinico-radiological outcomes after the Ganz approach [9]. Additionally, case reports have described open reduction via direct anterior approach (DAA) for bilateral symmetrical Pipkin type II fractures with satisfactory results [11].
However, controversies still exist. Trochanteric osteotomies have been performed in combination with posterior approaches for acetabular fractures, but reported outcomes are limited to single-center case series [16]. One study proposed a modified Gibson approach with trochanteric osteotomy for Pipkin type IV fractures, but it acknowledged the need for more prospective studies to determine an optimal surgical approach [18].
Arthroscopic-assisted percutaneous fixation has also been reported for Pipkin type II fractures, allowing for minimally invasive management, but the applicability of this technique to a wider range of cases remains uncertain [13]. Minimally invasive osteosynthesis approaches for distal femoral shaft fractures have been described [7], but their relevance to femoral head fractures is unclear.
Factors influencing the outcome of osteosynthesis after closed reduction of femoral neck fractures have been evaluated in young adult patients [14], but similar analyses for femoral head fractures are scarce. Furthermore, the long-term outcomes of osteosynthesis for femoral head fractures remain largely unexplored in the literature [15].
In conclusion, while surgical dislocation with trochanteric osteotomy has been utilized for the management of Pipkin II femoral head fractures [1], alternative approaches have also been described in the literature [9,11,13,20]. Further research, preferably through multicenter randomized controlled trials, is needed to establish the most appropriate surgical techniques for different types of Pipkin fractures and compare their long-term outcomes. Additionally, factors influencing the success of osteosynthesis in the context of femoral head fractures warrant further investigation.
Author's Resources & References
Search for Related Literature

Daniel B. Chan, MD
- United States ,
- Area of Specialty - Joint Replacement
- Position - Head of Department

Industry Sponsership
contact us for advertising opportunities






.jpeg)

User Discussion (1)
Dr Ed Oates
Impressive. Both the technical aspect of the surgical dislocation, as well as the elegance of the fixation. How did they fair medium/long term?
Healed at last follow-up at 1 year postop but haven’t seen the patient in a while…