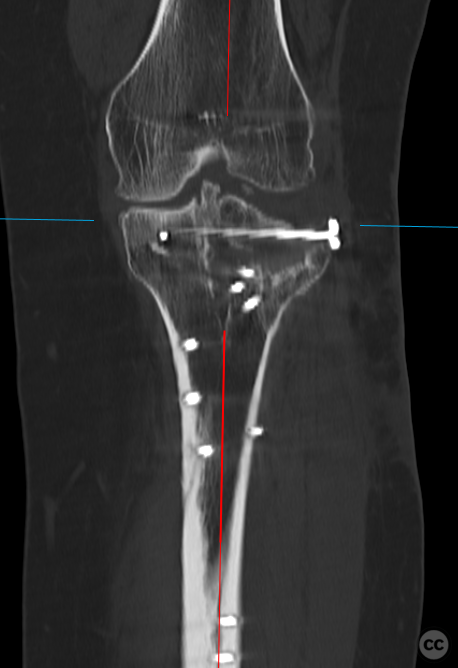
Schatzker 6 tibial plateau with lateral femoral epicondyle osteotomy
Score and Comment on this Case
Clinical Details
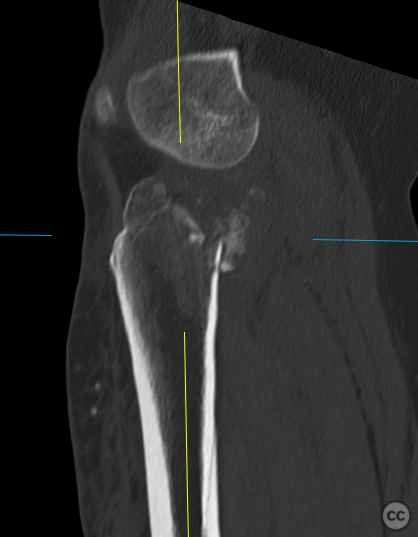
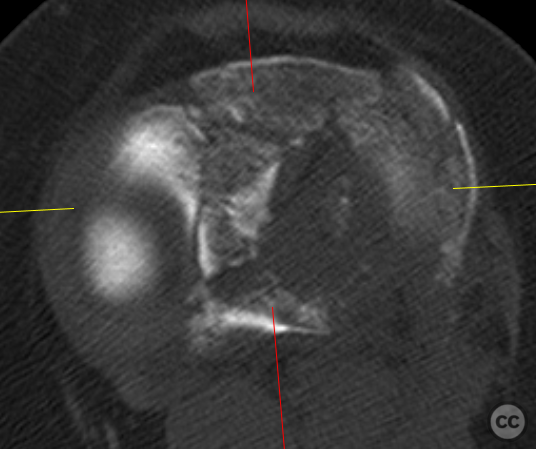
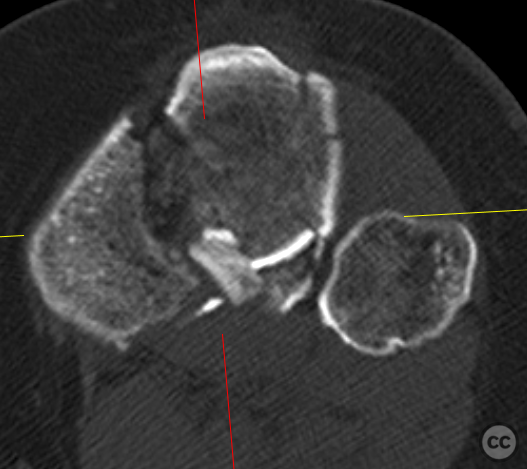
Clinical and radiological findings: A 40-year-old female pedestrian was struck by a car, resulting in a closed injury to her left knee. The patient, of short stature and overweight, presented with significant swelling and pain. Radiological assessment revealed a Schatzker VI / Kahn M5 / AO41B3.3 / Moore 2 fracture, indicating a complex tibial plateau fracture involving the lateral and medial condyles with significant articular surface involvement.
Preoperative Plan
Planning remarks: Given the complexity of the fracture, a multifaceted surgical approach was planned. The primary goal was to restore the articular surface and correct mechanical alignment while minimizing soft tissue disruption. The initial plan involved a lateral decubitus position transitioning to supine, utilizing both anterolateral and anteromedial approaches. Osteotomy was considered to facilitate exposure and reduction. Medially, the use of simple lag screws and buttress plating was anticipated, with the possibility of transitioning to a more extensive posteromedial plating depending on intraoperative findings.
Surgical Discussion
Patient positioning: The patient was initially positioned supine with a carbon roll under the thigh to facilitate near 360deg access around the knee.
Anatomical surgical approach: The surgical approach commenced laterally with an extensile incision to address the complex fracture pattern. A femoral epicondylar osteotomy was performed to improve visualization and access to the central- and posterolateral corner.
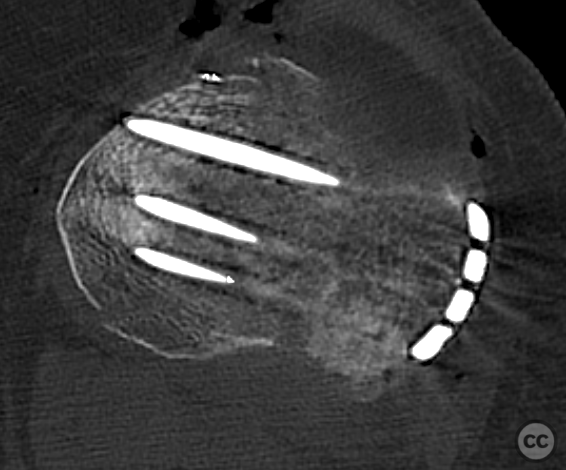
Operative remarks:The surgery was challenging due to the extensive soft tissue and poor visualization in the posterolateral corner. However, the extensile approach with epicondylar osteotomy allowed for successful reconstruction of the lateral column utilizing provisional inside-out K-wires and definitive PLLA Drill-Pins, supplemented by an anterolateral locking plate for column stabilization. The lateral meniscal tear and medial luxation were addressed through suture repair. Despite a residual defect in the lateral plateau, overall intraarticular congruity and mechanical axis were satisfactory.
Postoperative protocol: Postoperatively, the patient was placed on a non-weight-bearing to touch weight-bearing protocol for 10 weeks with a range of motion brace to limit varus forces. The meniscal repair protocol included restricted range of motion increments over 6 weeks.
Follow up: 2 years postop, a progressive loss of lateral column height, together with articular impaction have converged to elective ROH and planned TKA in ca 6-9 months
Orthopaedic implants used: Anterolateral locking plate with plate-based locked subchondral rafting screws, a minimally invasive percutaneous osteosynthesis (MIPO) medial locking plate, and PLLA Drill-Pins for articular surface reconstruction.
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisThe literature on risk factors for conversion to total knee arthroplasty (TKA) after tibial plateau fracture (TPF) presents a multifaceted picture where patient demographics, fracture characteristics, surgical techniques, and postoperative management converge to influence outcomes [1-12].
The overall conversion rate from treated TPFs to TKA is reported at approximately 5%, with certain subgroups exhibiting higher rates [1]. Identified risk factors include female sex, advanced age at the time of injury or surgery [2], low surgeon and hospital volume [9], previous infection related to tibial plateau repair surgery not correlating with prosthetic joint infection but influencing incision placement decisions during subsequent TKA [2], substantial preoperative fracture displacement [3], inadequate postoperative coronal and sagittal alignment of the tibia [3], obesity [10], varus malalignment of the lower extremity [11] as well as osteoporosis contributing towards inclination of the tibial plateau in postmenopausal women with OA knee [8].
Radiographic predictors such as initial gap greater than 8.5 mm and step-off over 6.0 mm are strongly associated with increased risk for conversion to TKA after TPF surgery according to multivariable analyses; however residual incongruity between 2-4 mm was not found significantly associated when compared with adequate reduction under 2 mm—indicating that small degrees of articular surface mismatch may be tolerated without accelerating progression towards arthroplasty within observed follow-up periods[3].
Furthermore, patients who consumed tobacco were more likely to require joint replacement following ORIF for tibial plateau fractures; younger patients tended toward osteochondral allograft (OCA) transplantation rather than conventional TKA when addressing posttraumatic arthritis[7]. This indicates that lifestyle factors can also play a role in long-term outcomes following these injuries.
It has been suggested that high-volume treatment centers exhibit lower rates of conversion to TKA suggesting potential benefits in regionalizing care for complex injuries like TPFs[9]. Additionally, it is posited that elderly patients do not inherently face poorer radiographic outcomes or higher complication rates compared against their younger counterparts after ORIF indicating suitability across ages if other risk factors are managed appropriately[4].
Lastly, spontaneous osteonecrosis/subchondral insufficiency fractures which commonly present alongside medial meniscal root tears can progress toward arthroplasty at notable rates especially among older individuals demonstrating baseline arthritis along with varus alignment issues further complicating prognosis even outside direct traumatic contexts such as acute TPFS[12].
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities





























Article viewed 1392 times
05 Feb 2024
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2024). Schatzker 6 tibial plateau with lateral femoral epicondyle osteotomy. Journal of Orthopaedic Surgery and Traumatology. Case Report 428460 Published Online Feb 05 2024.