Posterolateral Tibial Plateau Fracture with Meniscal Rupture
Score and Comment on this Case
Clinical Details
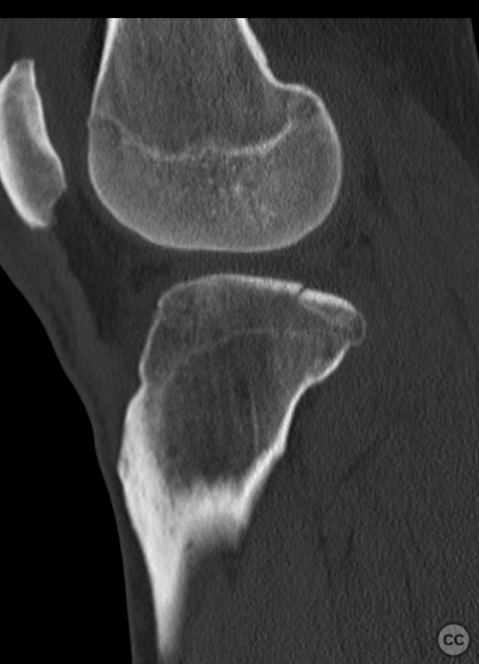
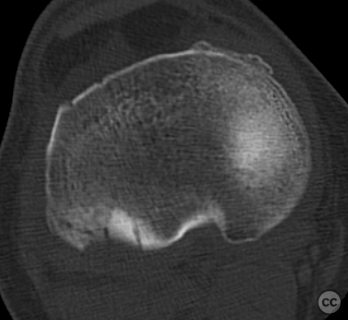
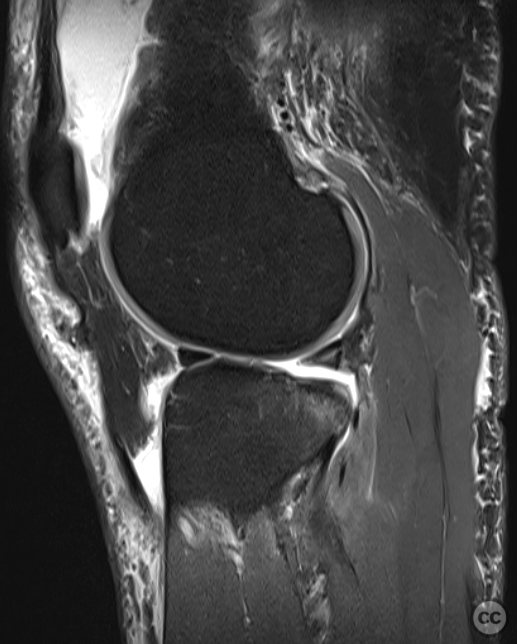
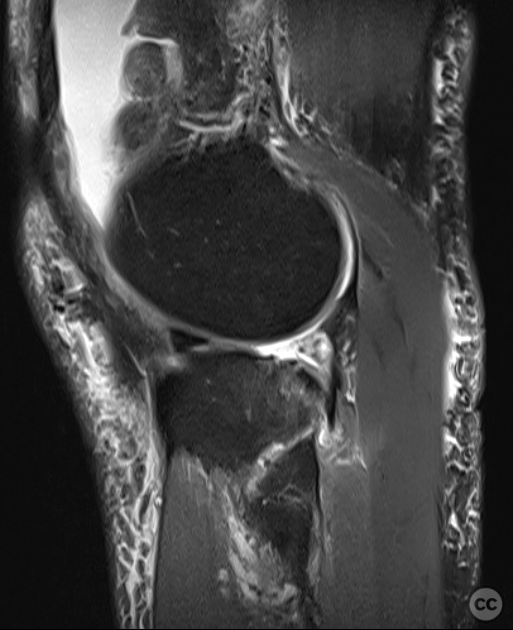
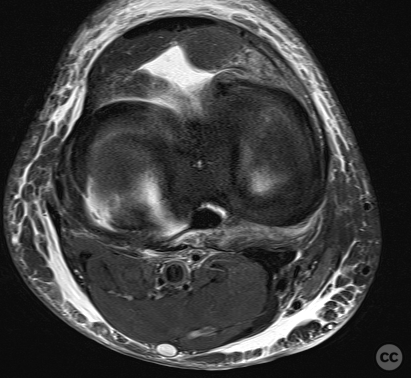
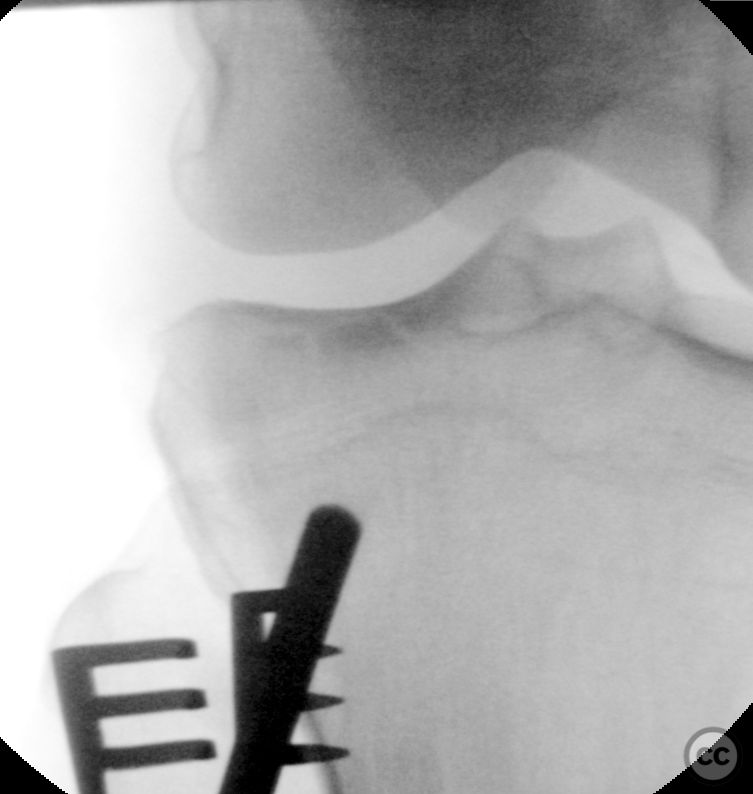
Clinical and radiological findings: A 47-year-old male presented 24 hours post-injury after stumbling and twisting his right knee while walking down two steps. The patient was able to bear full weight and reported minimal pain. Initial plain film X-rays suggested a posterolateral tibial plateau fracture. Subsequent CT imaging confirmed a 3-4mm far posterolateral impression fracture with not significant step-off. An opportunistic ambulant MRI demonstrated an extruded and defunctioned meniscus due to a complete posteior radial tear / rupture.
Preoperative Plan
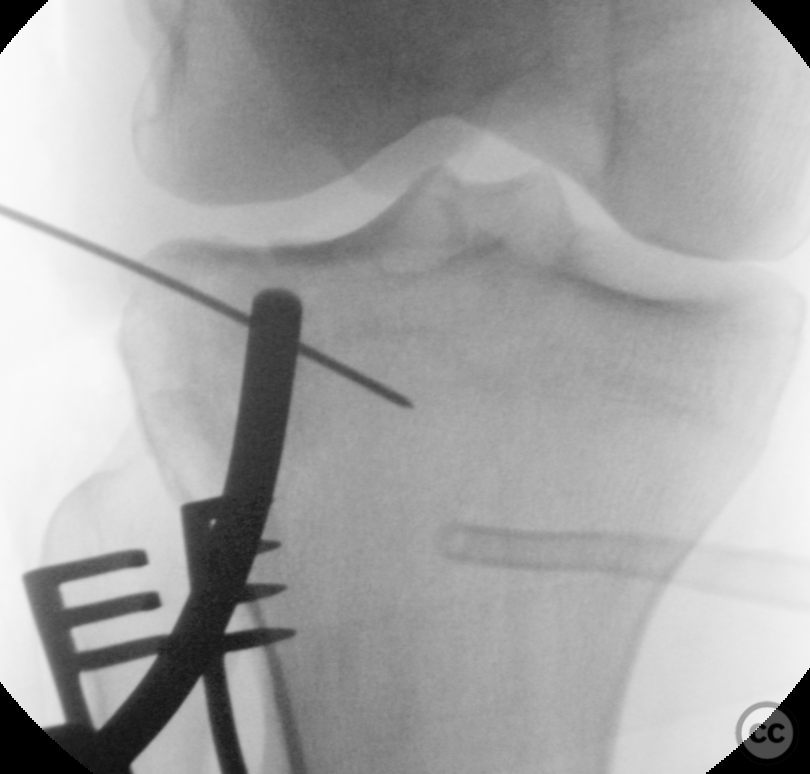
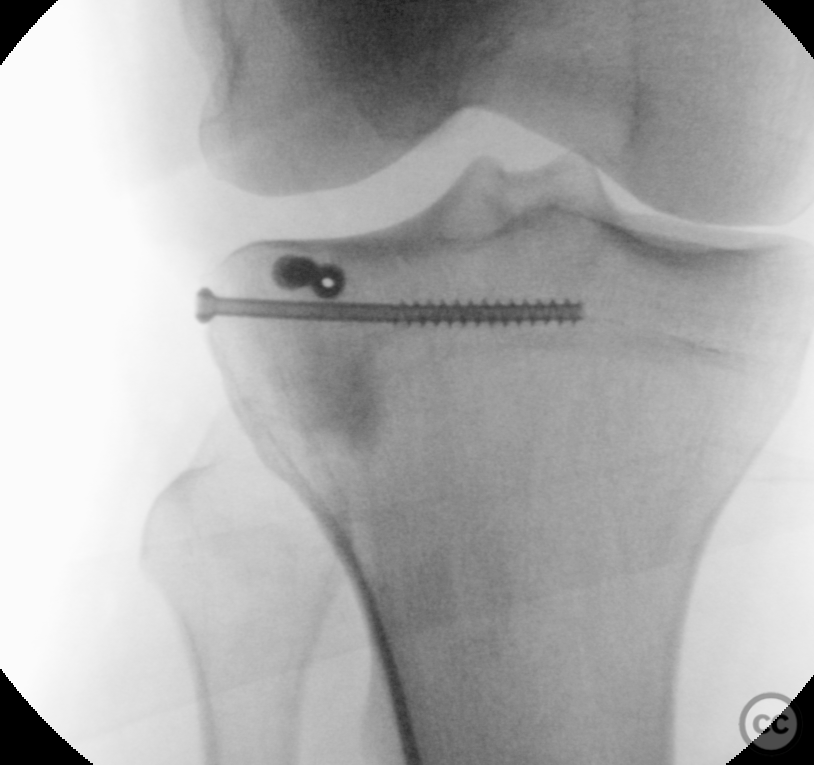
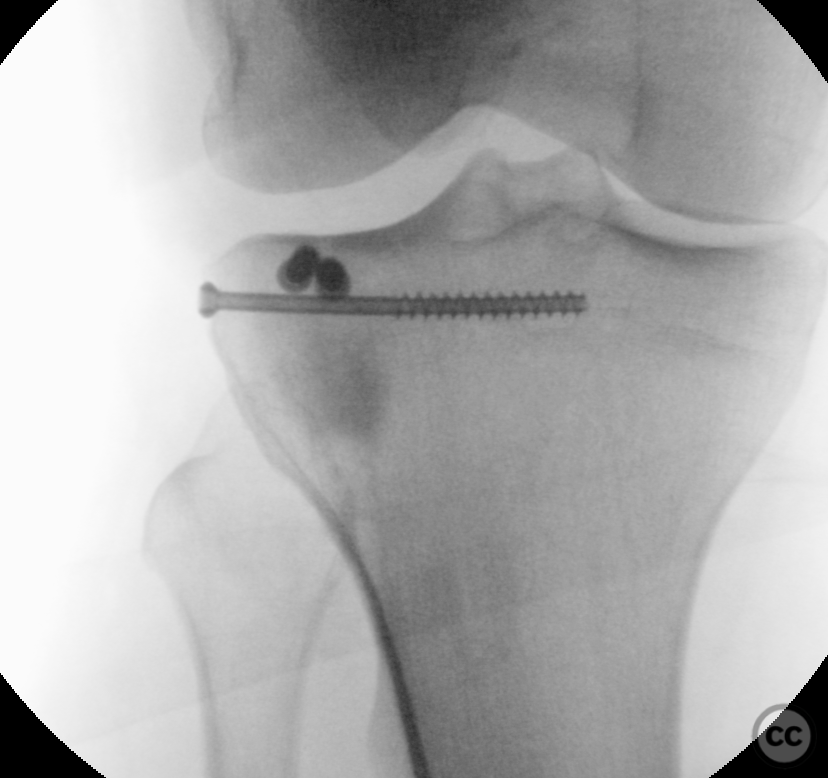
Planning remarks: The planned surgical approach involved an arthroscopically assisted procedure. The initial step was a knee arthroscopy to address the meniscal tear, followed by fluoroscopically guided minimally invasive reduction of the articular surface and defect filling. Stabilization was planned using a 4.0mm cannulated subchondral raft and 'jail-screw' technique.
Surgical Discussion
Patient positioning: Supine position with the affected leg placed in a leg holder to allow for arthroscopic access and fluoroscopic guidance.
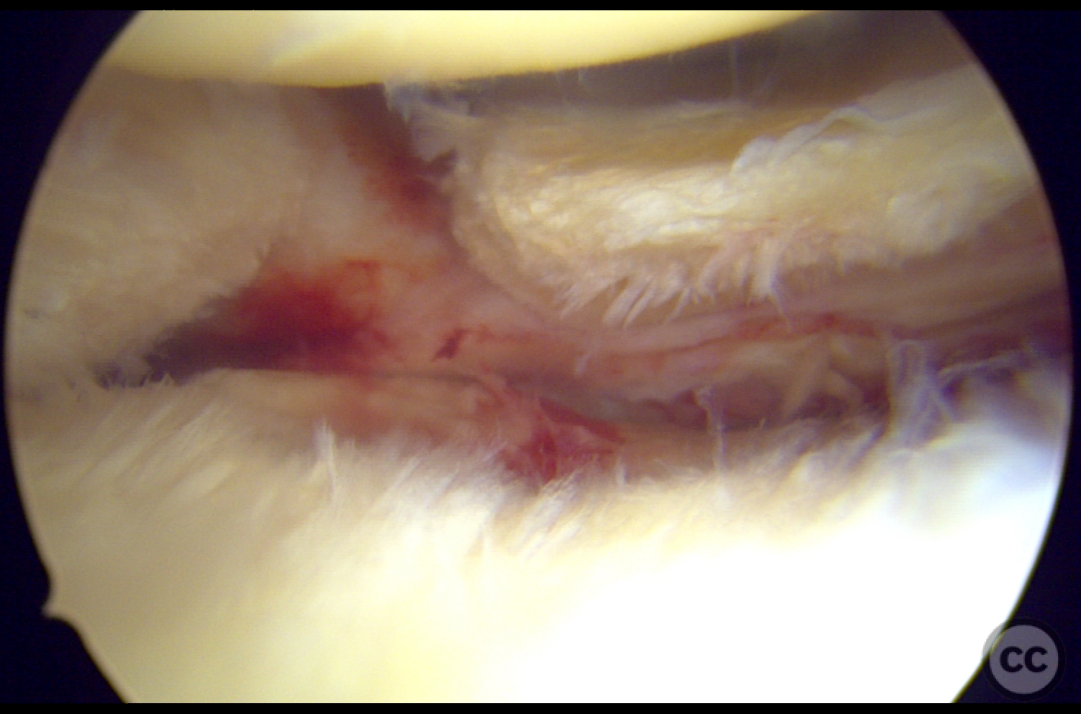
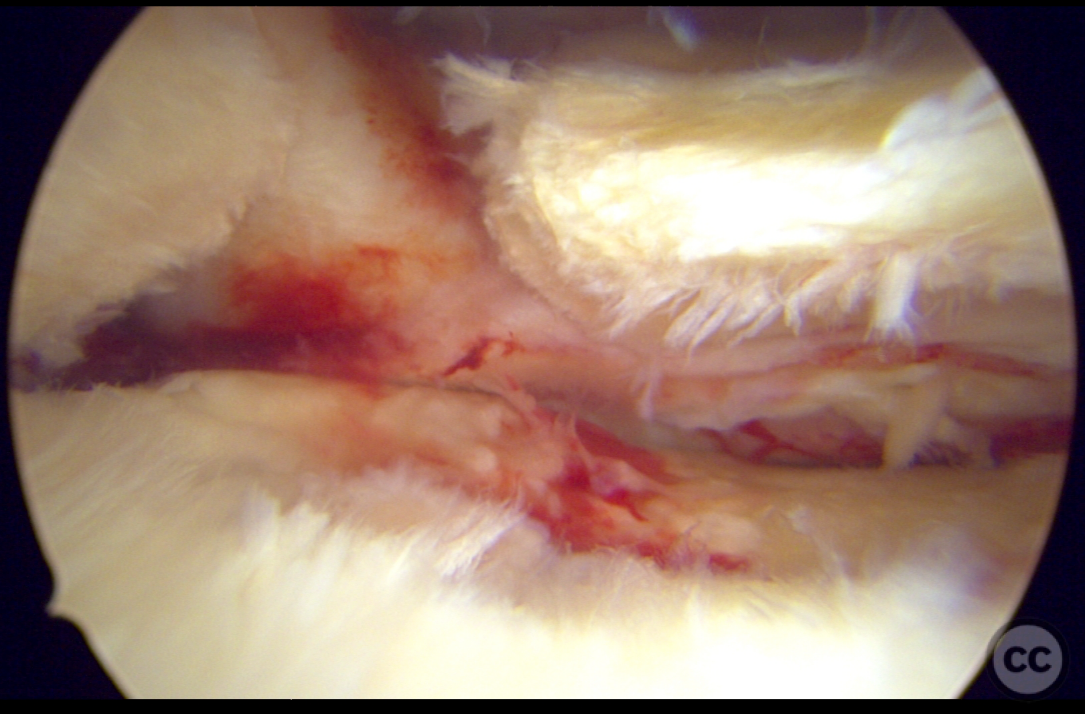
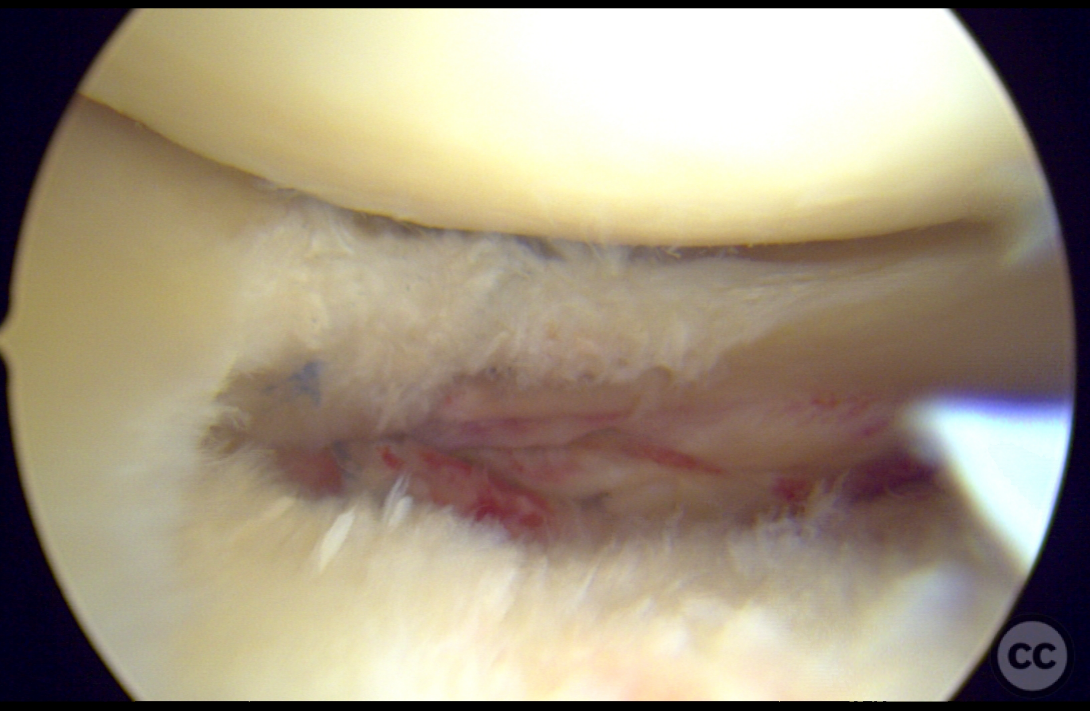
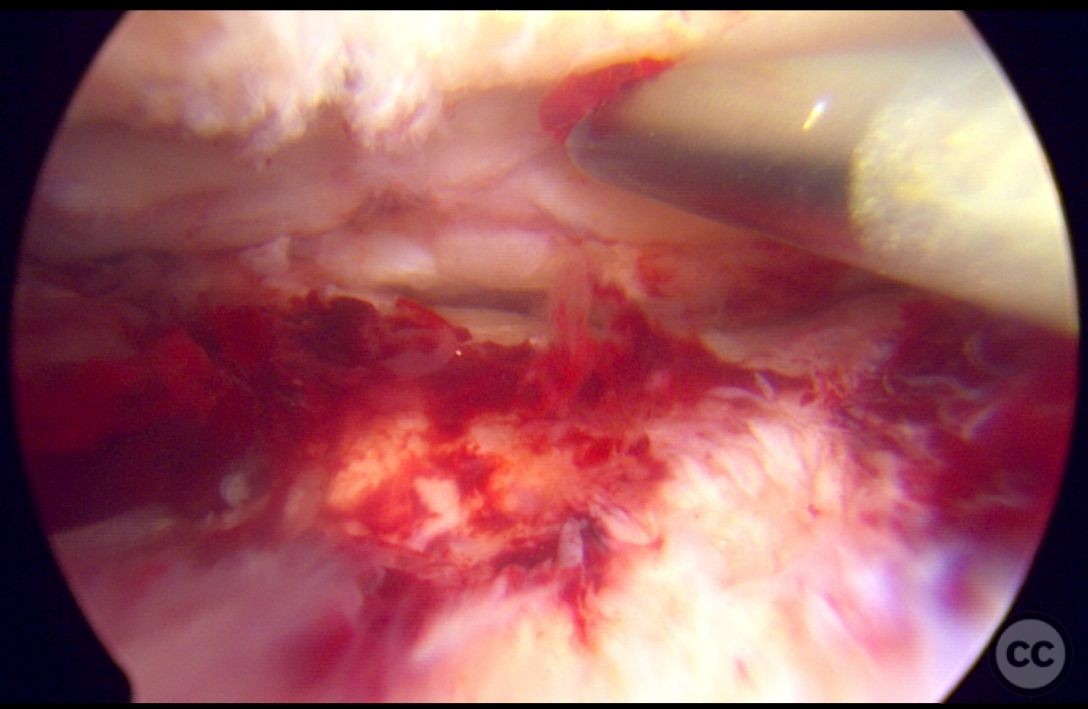
Anatomical surgical approach: A standard anterolateral portal was established for knee arthroscopy. The complete radial tear of the posterior meniscus overlying the fracture margin was identified. Five all-inside sutures were used to reduce and fix the tear, restoring ring tension. Following meniscal repair, a minimally invasive latteral approach was utilized under fluoroscopic guidance to tamp the articular surface and fill the defect. A 4.0mm cannulated subchondral raft and 'jail-screw' were then placed to support the articular surface.
Operative remarks:The complete radial tear of the posterior meniscus was successfully adapted and fixed with five all-inside arthrex sutures, restoring ring tension and function. Fluoroscopic guidance facilitated accurate reduction of the articular surface and defect filling with Vitoss. The subchondral raft and jail-screw provided stable foundation of the articular surface. Final arthroscopic inspection confirmed both the stability of the meniscal repair, togeter with the anatomic restoration of the surface - including posterior meniscal support.
Postoperative protocol: Postoperatively, the patient will be managed in a range of motion (ROM) brace limited to 30 degrees for 4 weeks, increasing to 60 degrees at 6 weeks, and 90 degrees at 8 weeks postop. Touch weight bearing will be maintained until 8 weeks, followed by progression to full weight bearing by 10 weeks.
Follow up: Not specified
Orthopaedic implants used: - Arthrex Fiberstitch all-inside meniscal sutures - 4.0mm cannulated screws - Vitoss bone graft substitute
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities








Article viewed 1052 times
07 Jun 2024
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2024). Posterolateral Tibial Plateau Fracture with Meniscal Rupture. Journal of Orthopaedic Surgery and Traumatology. Case Report 44318305 Published Online Jun 07 2024.