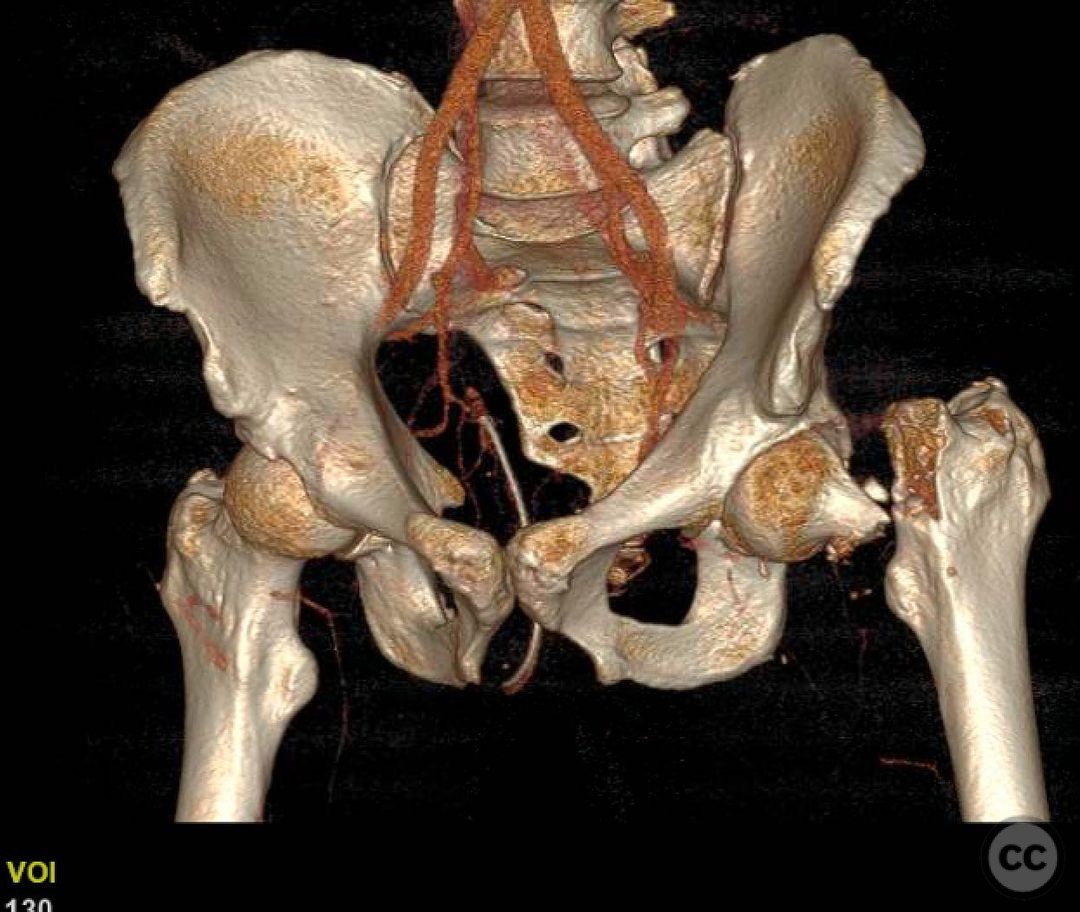
Vertical displaced femoral neck fracture
Score and Comment on this Case
Clinical Details
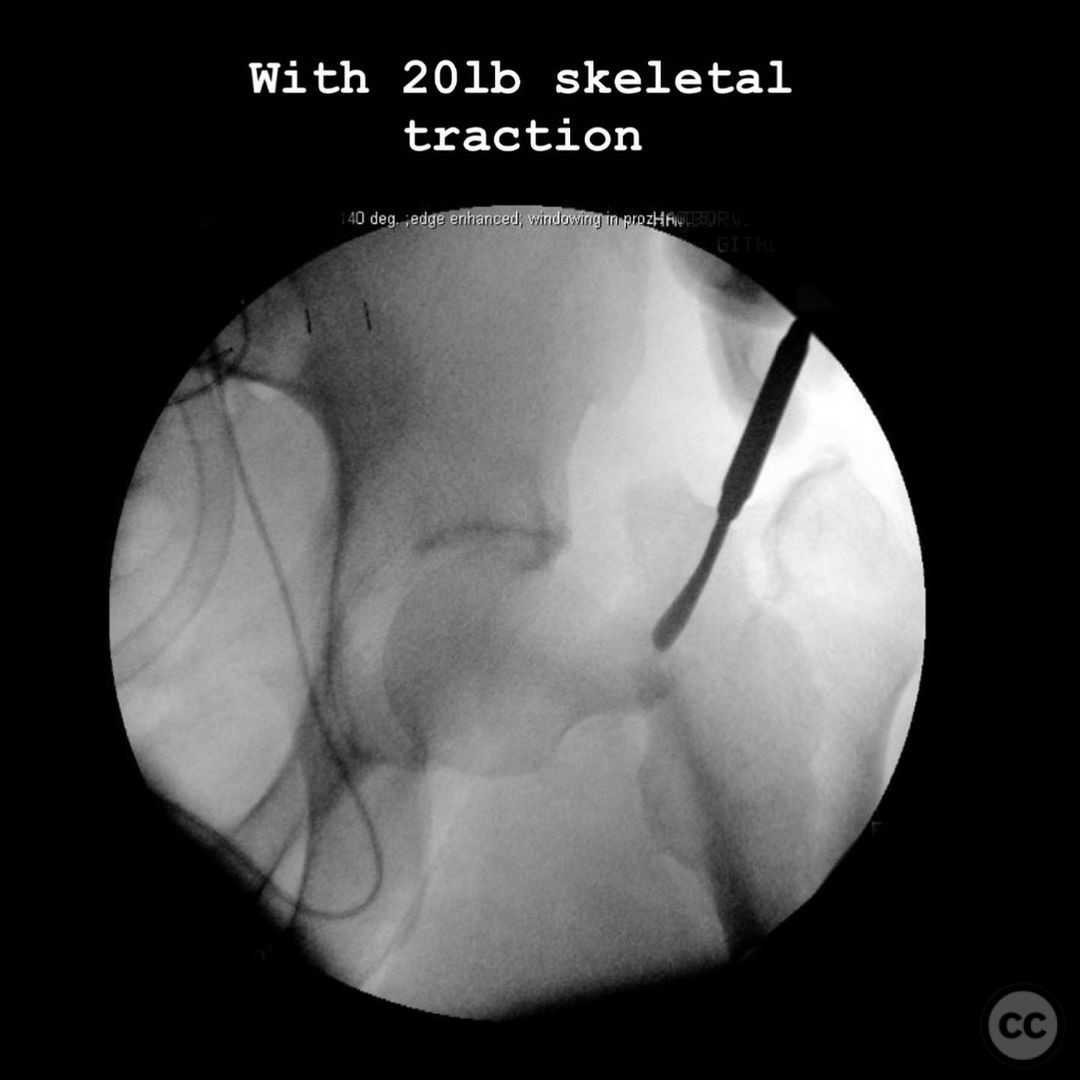
Clinical and radiological findings: 41yo, high speed motorcycle accident. This is a high energy injury in a young male. The displacement pattern is unusual. Typically there is some shortening, varus, and retro version, but the fragments remain in contact. In this pattern the fragments are in different zip codes. This is worrisome for AVN risk, but also may effect the surgical strategy. How? there has to be a reason for that degree of displacement. A traction view may give you more information (see the second image). With traction, nothing improves. Usually traction helps via ligamentotaxis, at least to some degree. Here, nothing happened. At a minimum, the traction view tells you an open reduction is 100% required if you are going to fix this- a traction table reduction won’t work. Which brings us to the question of fix vs replace. This is an individual discussion with the patient- an honest appraisal of the risks and benefits of each. While this patient’s risk for AVN is elevated compared to other displaced femoral neck fractures, we don’t know what it is. And many people live with hip AVN for years without significant symptoms. Native parts are better than fake parts in young people until the young person cannot live the native part anymore. So this guy gets a proper fix, and time.
Preoperative Plan
Planning remarks: Plan
Surgical Discussion
Operative remarks:A fix means Heuter approach for reduction, subvastus approach for implant placement. I do the heuter first- a word of caution- with this much deformity, the approach may become less straightforward as things aren’t where they normally are. I went straight to a rectus tenotomy because the fracture exit was very cranial and the patient was quite muscular. Hard fracture- load the boat in your favor. Usually I don’t do one for femoral necks. Once the fracture is exposed, do the subvastus approach and preload a handful of 2.0 and 2.4mm wires. That way you’re ready to rock once you have the reduction. The worst thing is to struggle to get a reduction, then do a lateral approach only to find you’ve lost the reduction. Hard fracture- load the boat in your favor.
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisA deeper understanding of the pathoanatomy of vertical femoral neck fractures in young patients is crucial for improving treatment decisions, including reduction and fixation. Sarfani et al. utilized advanced 2D and 3D computed tomography to better describe fracture patterns and pathoanatomy in this population[2]. Finite element analysis has been widely employed to assess the stability of femoral neck fracture fixation. Samsami et al. examined the stability of fracture fixation using finite element models and simulating progressive consolidation for vertical femoral neck fractures, concluding that sliding hip screws provided the best overall stability[3].
Guimarães et al. proposed a closed fixation strategy using a transverse cancellous lag screw for vertical femoral neck fractures in young adults, showing promising results, though further studies are needed to validate this technique[4]. Huang et al. evaluated the effect of closed reduction and internal fixation with three different screw configurations in acute completely displaced femoral neck fractures, reporting that although complications occurred, the technique provided satisfactory results[5]. Samsami et al. compared three fixation methods for femoral neck fractures in young adults, suggesting that the choice of fixation method should be based on the fracture type and patient-specific factors[6].
Teng et al. evaluated the Femoral Neck System (FNS) in the treatment of Pauwels type III femoral neck fractures, finding that the FNS had higher maximum displacement compared to other methods, indicating the need for further optimization of the FNS design[7]. Li et al. conducted a finite element analysis of a medial anatomical buttress plate for displaced femoral neck fractures, indicating that the buttress plate might provide better stability in vertical fractures[8]. Giordano et al. assessed a locking autocompression screw model for Pauwels type-3 femoral neck fractures, revealing that the construct provided satisfactory mechanical performance, but further studies are necessary to support its clinical application[9].
In conclusion, various fixation methods have been studied to address the challenge of treating vertical displaced femoral neck fractures in young patients. Advanced imaging techniques and computational models have been employed to understand the pathoanatomy and stability of fracture fixation. While some promising results have been reported, further research is needed to establish the optimal treatment strategy for this patient population.
References:
[2] https://pubmed.ncbi.nlm.nih.gov/34101703/
[3] https://pubmed.ncbi.nlm.nih.gov/31203740/
[4] https://pubmed.ncbi.nlm.nih.gov/29145961/
[5] https://pubmed.ncbi.nlm.nih.gov/21162504/
[6] https://pubmed.ncbi.nlm.nih.gov/26500470/
[7] https://pubmed.ncbi.nlm.nih.gov/35839002/
[8] https://pubmed.ncbi.nlm.nih.gov/31455504/
[9] https://pubmed.ncbi.nlm.nih.gov/36135010/
Search for Related Literature

orthopaedic_trauma
- United States , Seattle
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities










Article viewed 2038 times
15 Jan 2023
Add to Bookmarks
Full Citation
Cite this article:
Surname, Initial. (2023). Vertical displaced femoral neck fracture. Journal of Orthopaedic Surgery and Traumatology. Case Report 47035380 Published Online Jan 15 2023.