Revision Plate Osteosynthesis for Humeral Shaft Non-Union Post Intramedullary Nailing
Score and Comment on this Case
Clinical Details
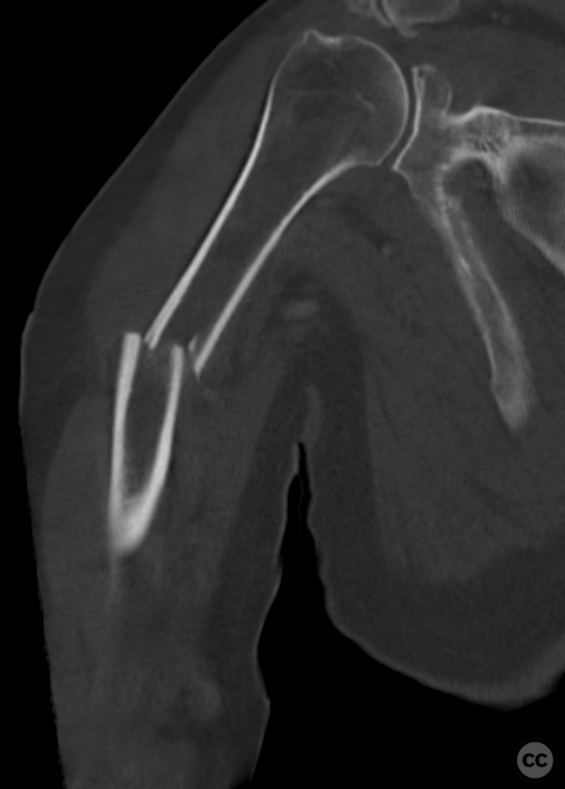
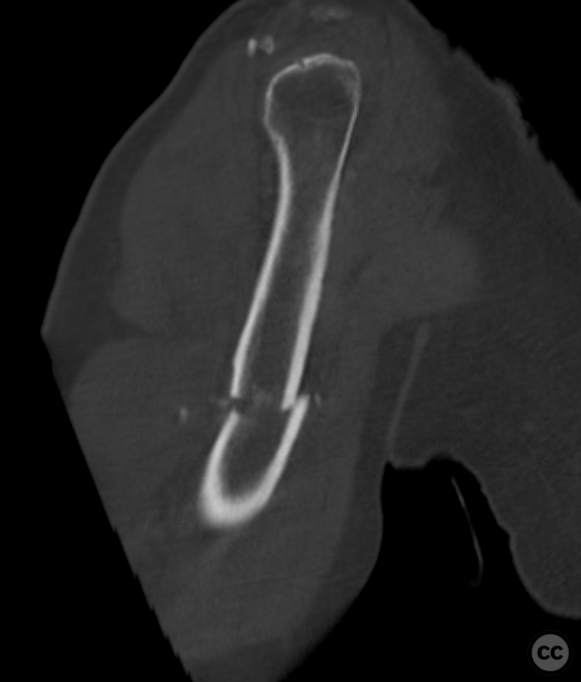
Clinical and radiological findings: An 82-year-old male sustained a minimally comminuted transverse fracture of the right humeral midshaft following a 3-meter fall. Given the patient's age, the decision was made to proceed with primary surgical fixation to facilitate early mobility and independence, despite the potential for conservative management. This Initial management with intramedullary nailing led, however, to a symptomatic hypertrophic non-union.
Preoperative Plan
Planning remarks: The preoperative plan included removal of the existing intramedullary nail followed by open reduction and internal fixation with plate osteosynthesis. An aggregate anterolateral approach to the humeral shaft was planned for comprehensive access for removal of Hardware and revision of the fracture site.
Surgical Discussion
Patient positioning: Semi-beach chair position with the right shoulder at the table edge, utilizing a spider positioner for stabilization.
Anatomical surgical approach: Initial appraoch was integrated a proximal deltoid split interval, utilising the original surgical scar, and extended distally in an 'S' shape to integrate an aggregate anterolateral approach.
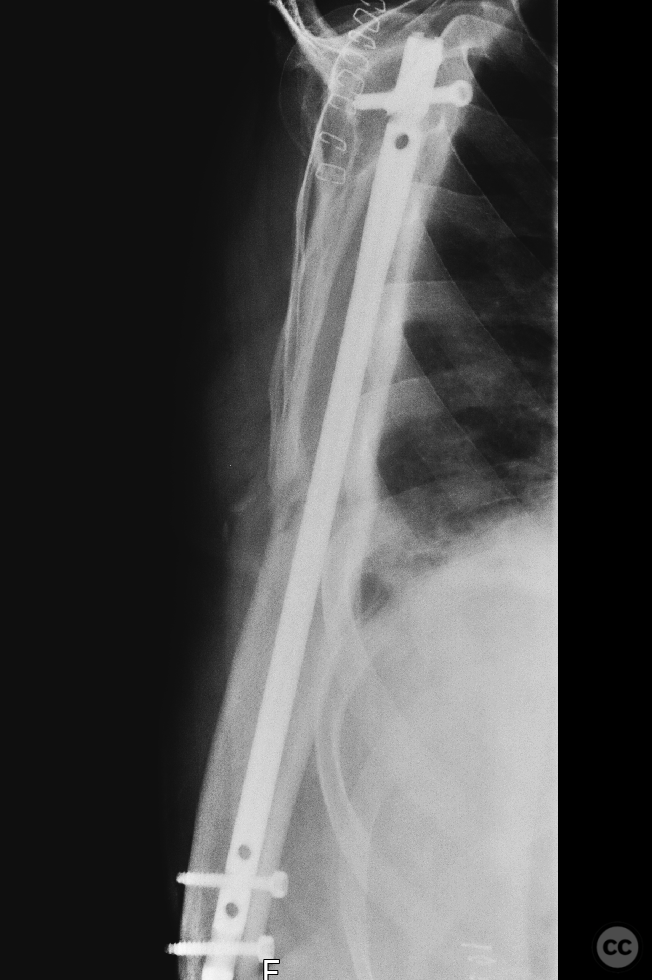
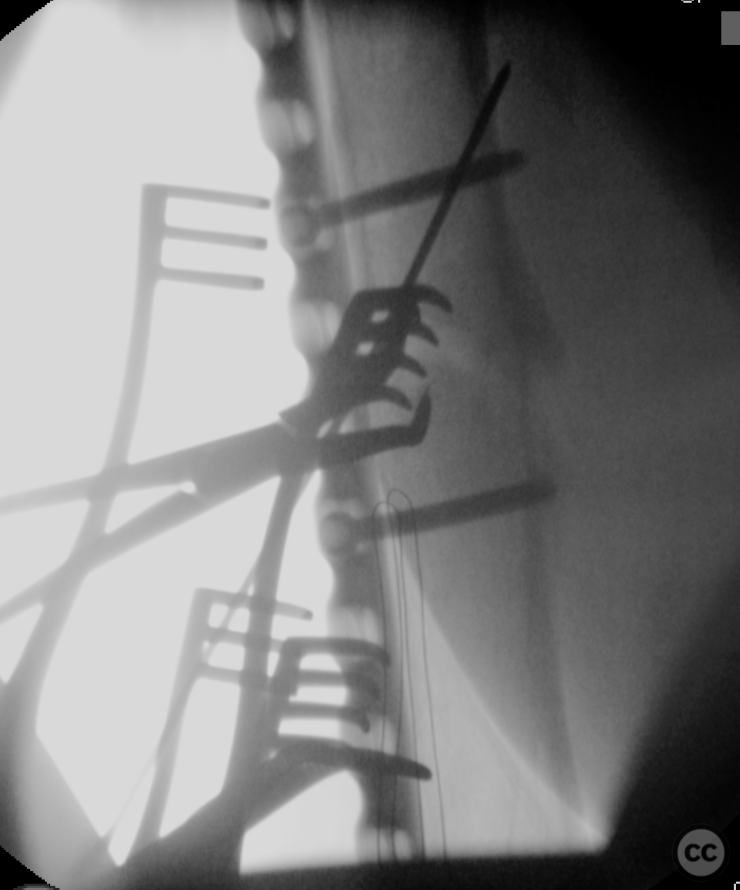
Operative remarks:Hardware removal involved careful dissection around the rotator cuff and greater tuberosity, followed by extraction of the intramedullary nail and locking screws under fluoroscopic guidance. The rotator cuff was found to be avulsed from the tuberculum with minimal retraction. A 3.5-millimeter corkscrew anchor was used for rotator cuff reattachment. The hypertrophic non-union site was addressed through debridement and preparation for plate osteosynthesis including subperiosteal elevation of the anterior aspect of the deltoid insertion with careful preservation of the radial nerve encapsulated in scar tissue. A 10-hole NCB plate was secured with bicortical screws, generating excellent compression at the non-union site
Postoperative protocol: Not specified
Follow up: Not specified
Orthopaedic implants used: 3.5mm Arthrex titanium corkscrew anchor, 10-hole Zimmer NCB plate
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisDespite advancements in surgical techniques and implant designs, achieving optimal results remains challenging due to the complexity of fracture patterns, patient-specific factors, and potential complications [1][2][3].
Intramedullary nailing has been widely adopted as a viable option for treating humeral shaft fractures due to its minimally invasive nature and the biomechanical stability it provides [4]. However, concerns regarding nonunion rates have prompted investigations into factors influencing union outcomes post-IMN.
Nonunion rates after IMN vary across studies but are generally reported within a range suggesting comparable efficacy between IMN and other fixation methods such as plate osteosynthesis [5][6]. Amer et al.'s systematic review highlighted no significant difference in nonunion rates between plating (1.8%) versus nailing (3.9%), though they noted an increased risk of iatrogenic radial nerve injury with plating [7]. This finding underscores the importance of technique refinement and surgeon experience in minimizing complications associated with each method.
Several factors contribute to the risk of nonunion following IMN. Patient-related factors include advanced age, smoking status, comorbidities like diabetes mellitus or osteoporosis that impair bone healing capacity [8]. Fracture-related variables encompass comminution degree, fracture site displacement severity at presentation—particularly oblique fractures near the proximal third—and open versus closed fracture status [1][9].
Surgical technique also plays a pivotal role; improper nail size selection or inadequate stabilization can lead to micromotion at the fracture site impeding bone healing processes leading towards nonunion development [10]. The necessity for distal locking remains debated; Egrise et al.'s study suggested that distal locking might not be required for all cases if primary stability is achieved through proper nail impaction within the medullary canal except certain distal third fractures where it may still be necessary [11].
Treatment strategies for addressing established nonunions involve rigorous debridement back to healthy bleeding bone edges followed by stable fixation often combined with autologous bone grafting or alternative biologic enhancers aimed at stimulating osteogenesis at the nonunion site [12][13].
In conclusion, while intramedullary nailing offers many advantages including preservation soft tissue envelope integrity around humerus allowing early mobilization post-operatively; careful consideration must be given towards optimizing both patient selection surgical approach minimize risks associated particularly concerning issue such as nonunions which despite being relatively infrequent when they do occur present significant challenges both patients surgeons alike necessitating sometimes complex revision procedures ensure successful outcome ultimately achieved.
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities












User Discussion (1)
Guest User
What size nail was used to begin with? Was nail too thin for the canal which led to kind of instability?
gsgg
guest user comment
registered user comment