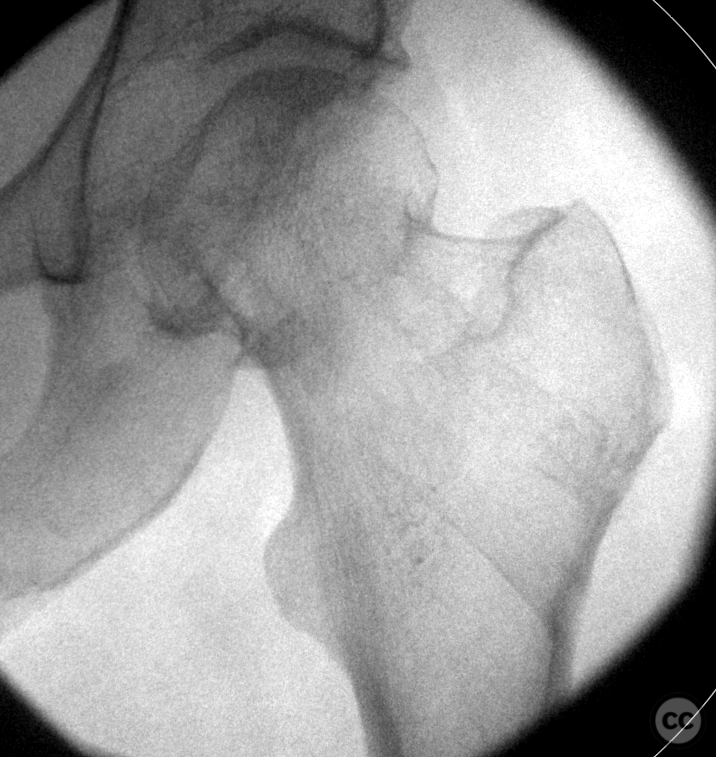
Garden I Subcapital Femoral Fracture in a 56yo Female
Score and Comment on this Case
Clinical Details
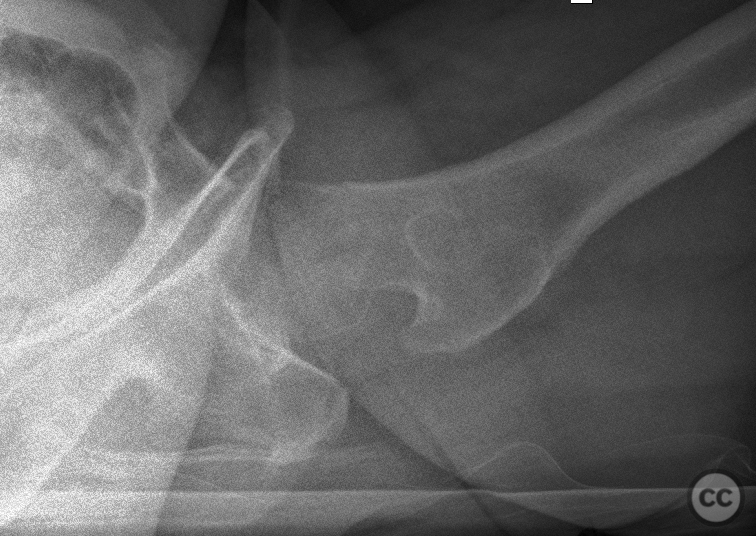
Clinical and radiological findings: A 56-year-old female, with an above-average fitness level and no significant past medical history, presented after a bicycle fall injuring her left side. Clinically, she exhibited an externally rotated left leg with an inability to weight bear. Initial radiographs in the Emergency Department revealed a Garden I subcapital femur fracture. Although a true lateral view was not obtained, there was an estimation of posterior inclination of the fracture at approximately 20-25 degrees.
Preoperative Plan
Planning remarks: Given the patient's desire to avoid trauma arthroplasty, a closed reduction followed by percutaneous cannulated screw fixation was planned. The goals were to achieve near-anatomic reduction of the fracture while minimizing soft tissue disruption and preserving blood supply to the femoral head.
Surgical Discussion
Patient positioning: The patient was positioned supine on a traction table allowing controlled axial traction and derotation under fluoroscopic guidance
Anatomical surgical approach: Under C-arm fluoroscopy guidance, a minimally invasive approach was used through a trans vastus window over the lateral aspect of the thigh.
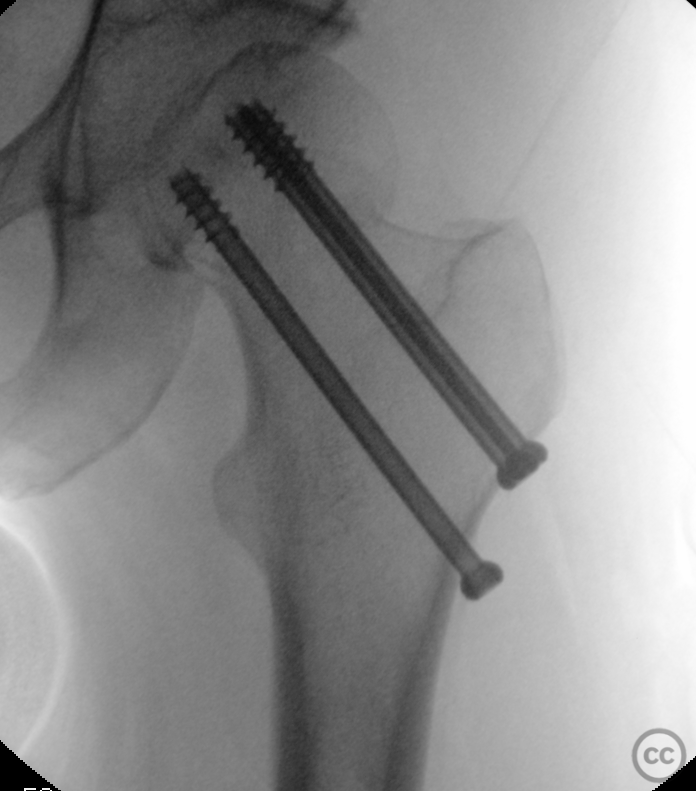
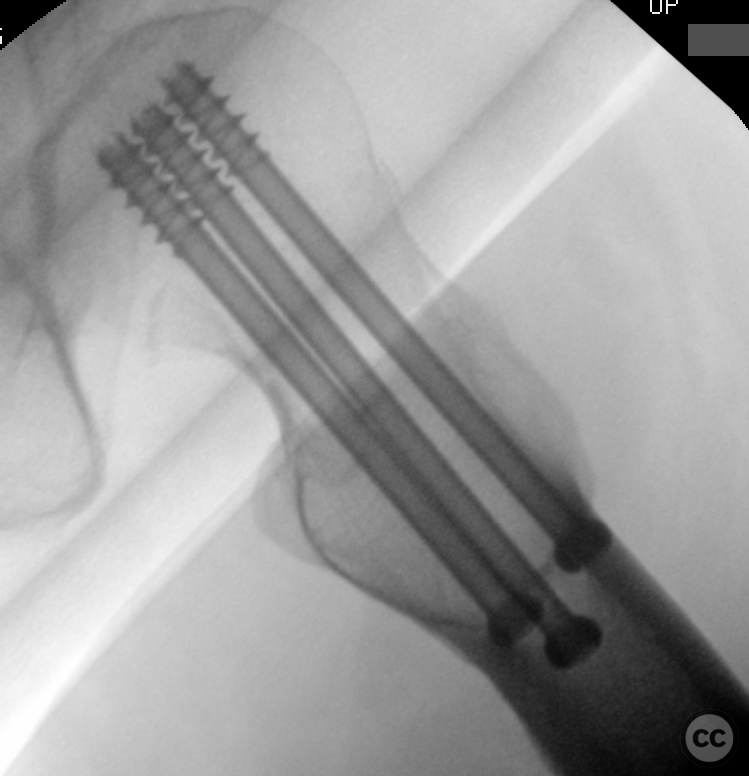
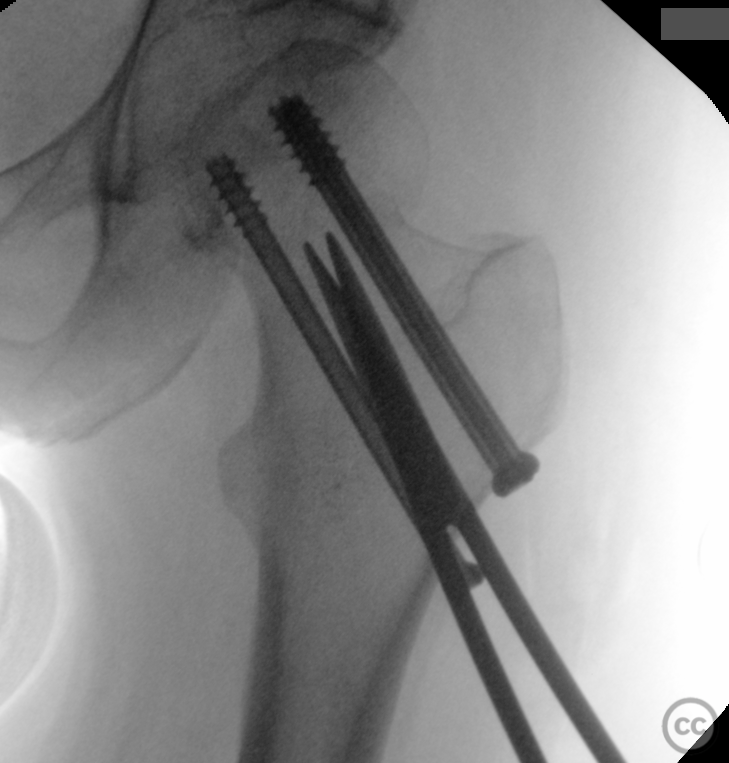
Operative remarks:Under C-arm fluoroscopy guidance, axial tension and derotation were applied to achieve near-anatomic reduction of the fracture. Following successful closed reduction, guide wires were inserted under fluoroscopic control to ensure proper alignment and length. Subsequently, three 7.3mm cannulated screws were introduced over these wires - one screw was positioned along the calcar femorale region to provide inferior cortical support (the most inferior calcar screw), while two additional screws were placed superiorly. Additionally, a capsulotomy was performed for decompression of intracapsular hematoma that could potentially increase pressure within the hip joint and compromise blood flow to the femoral head.
Postoperative protocol: The patient was advised touch weight bearing (TWB) for six weeks postoperative. At two years post-operation, hardware removal was conducted as pictured. Followup: The patient achieved pain-free ambulation without Trendelenburg gait; however, some abductor weakness compared to the contralateral side was noted, but did not limit daily nor sporting functions significantly due to her high pre-injury fitness level.
Orthopaedic implants used: Three 7.3mm cannulated screws placed in an inverted triangle configuration.
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisThe management of non-displaced neck of femur fractures remains contentious, with options including screw fixation and joint replacement (either hemiarthroplasty or total hip arthroplasty). A critical synthesis of the literature reveals nuanced outcomes dependent on patient demographics, fracture characteristics, and surgical intervention specifics. Wani et al. conducted a prospective cohort study (Level II) comparing internal fixation with cannulated screws versus total hip arthroplasty in patients aged between 60-80 years with displaced femoral neck fractures [1]. They reported superior functional outcomes as measured by Harris hip scores in the arthroplasty group at various follow-up intervals up to 18 months post-surgery [1]. However, McKinley and Robinson's matched-pairs case-control study (Level III) highlighted that early salvage total hip arthroplasty following failed internal fixation resulted in higher complication rates compared to primary arthroplasty [3]. Jettoo and James’s large-scale database analysis (Level III) found multiple screw fixation had shorter hospital stays but higher conversion rates to hemiarthroplasty or THA compared to dynamic hip screw (DHS) fixation [2]. Parker's pilot randomised trial among elderly men indicated that cemented hemiarthroplasty was associated with fewer reoperations compared to internal fixation using Targon Femoral Plate for displaced intracapsular fractures [4]. In contrast, Parker et al.’s comparison between internal fixation for undisplaced intracapsular fractures versus hemiarthroplasty for displaced fractures revealed benefits such as shorter operation time and reduced peri-operative complications favoring internal fixation [5]. Warschawski et al.'s comparative study showed no significant differences in complication rates or clinical outcomes when treating nondisplaced intracapsular hip fractures with either dynamic locking plate or simple cannulated screws [6]. Talboys et al.’s retrospective cross-sectional study suggested that total hip replacement might be more favorable than internal fixation regarding function and pain relief for patients aged 50-75 years suffering from displaced intracapsular fractures; however they noted no significant difference for undisplaced fracture treatment modalities [7]. García-Alvarez et al.'s prospective study identified risk factors predisposing infection postoperatively after Thompson arthroplasty for subcapital hip fracture but did not compare different surgical interventions directly related to our query [8]. Mouzopoulos et al., through their randomized division into three groups receiving different surgical treatments for displaced subcapital hip fracture over age 70 years old found better functional results after four years follow-up favoring total arthroplasties over both hemi-arthroplasties and internal fixations using Richards plates screws[9]. These findings collectively suggest an individualized approach considering patient age, activity level, comorbidities alongside specific fracture patterns is crucial when deciding on optimal management strategy between screw fixation versus joint replacement.
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities




Article viewed 677 times
02 Feb 2024
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2024). Garden I Subcapital Femoral Fracture in a 56yo Female. Journal of Orthopaedic Surgery and Traumatology. Case Report 48698488 Published Online Feb 02 2024.