Septic Nonunion of Subtrochanteric Femur Fracture with Hardware Failure
Score and Comment on this Case
Clinical Details
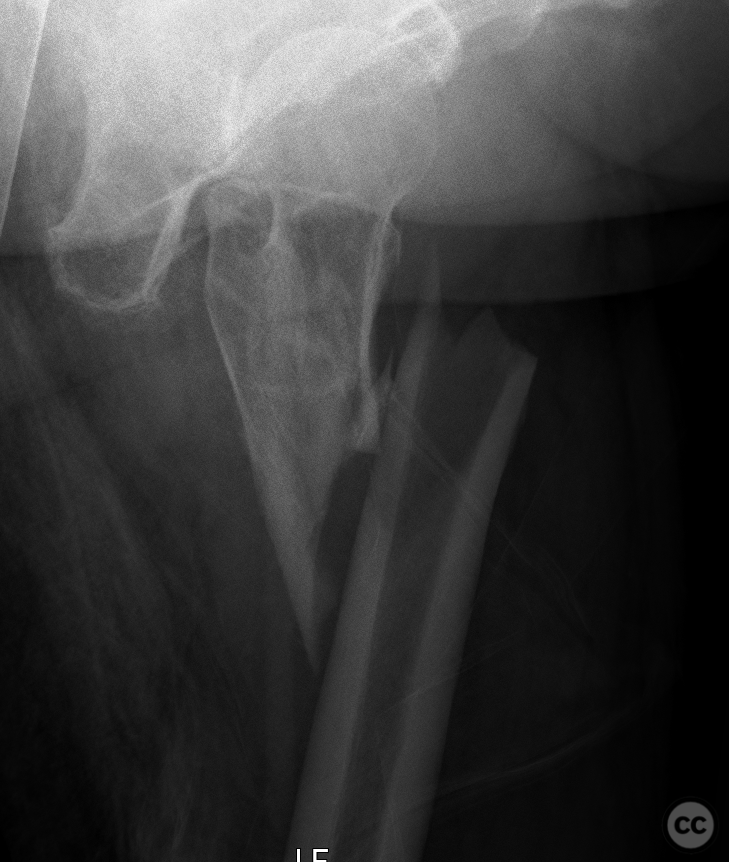
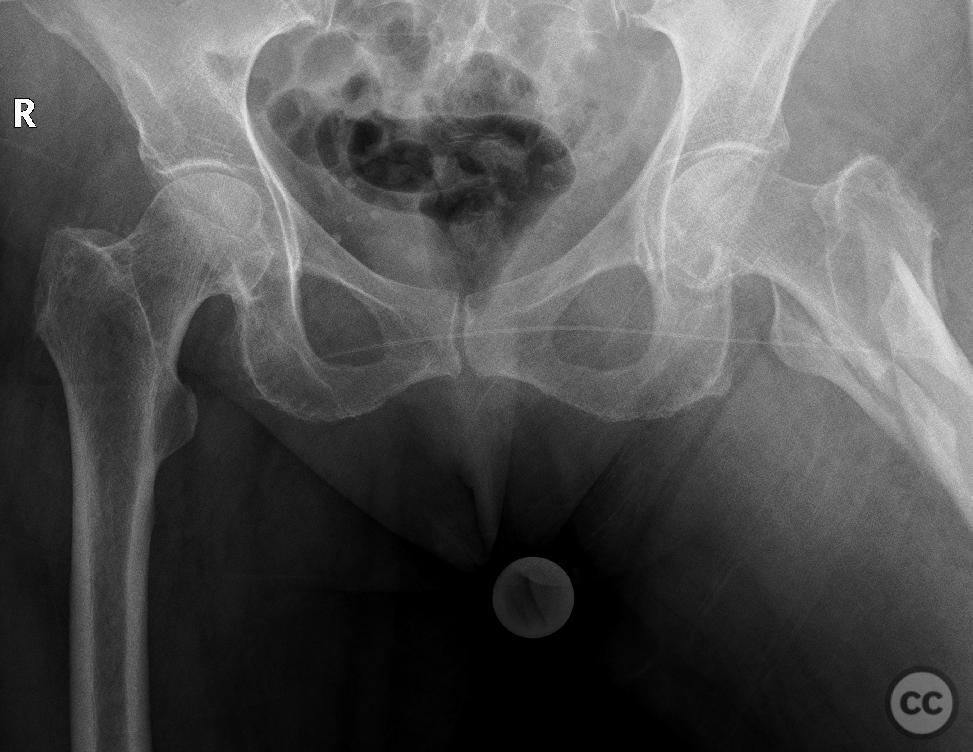
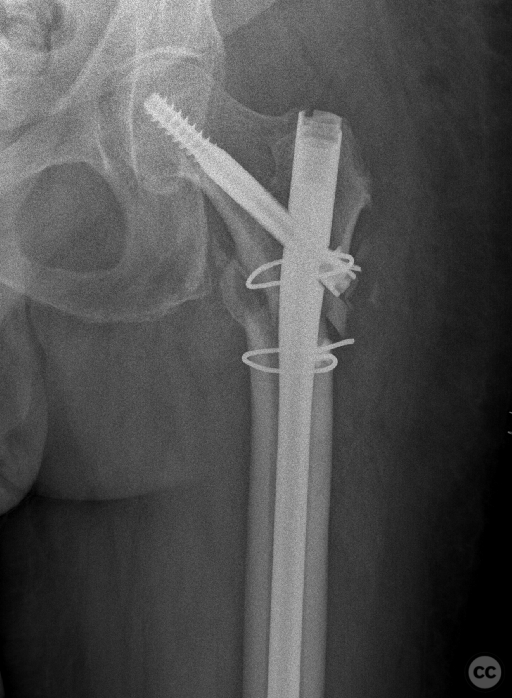
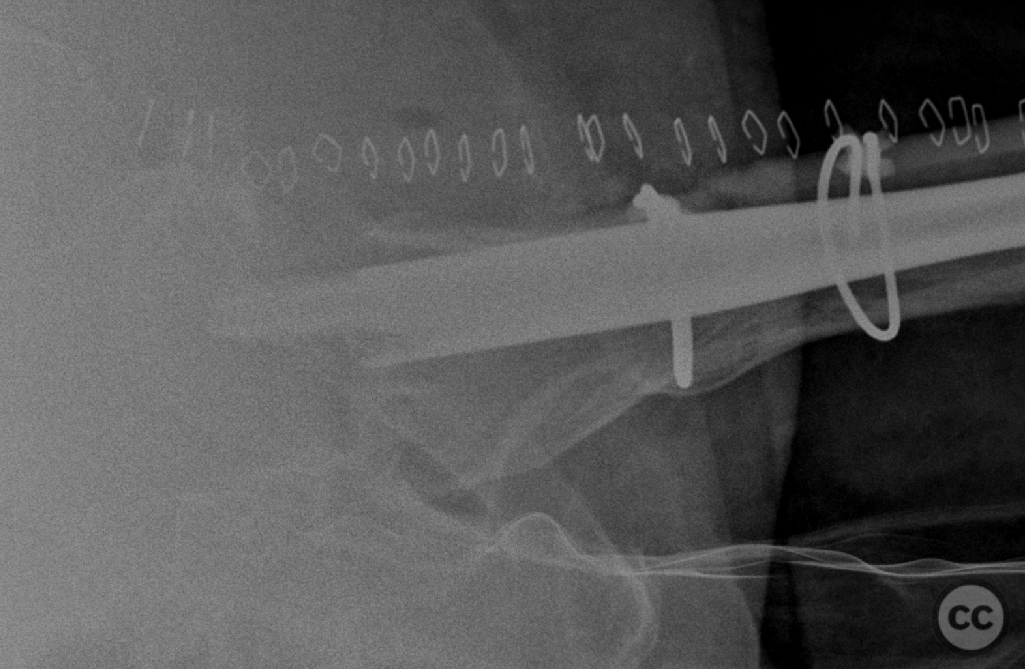
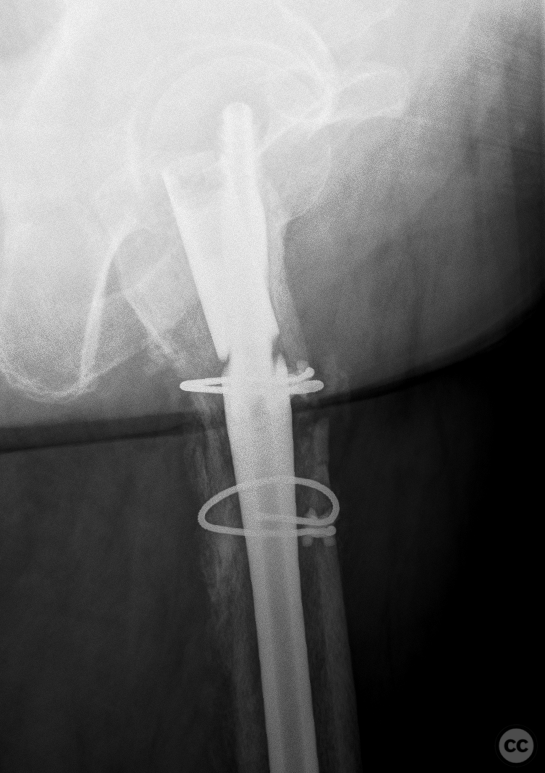
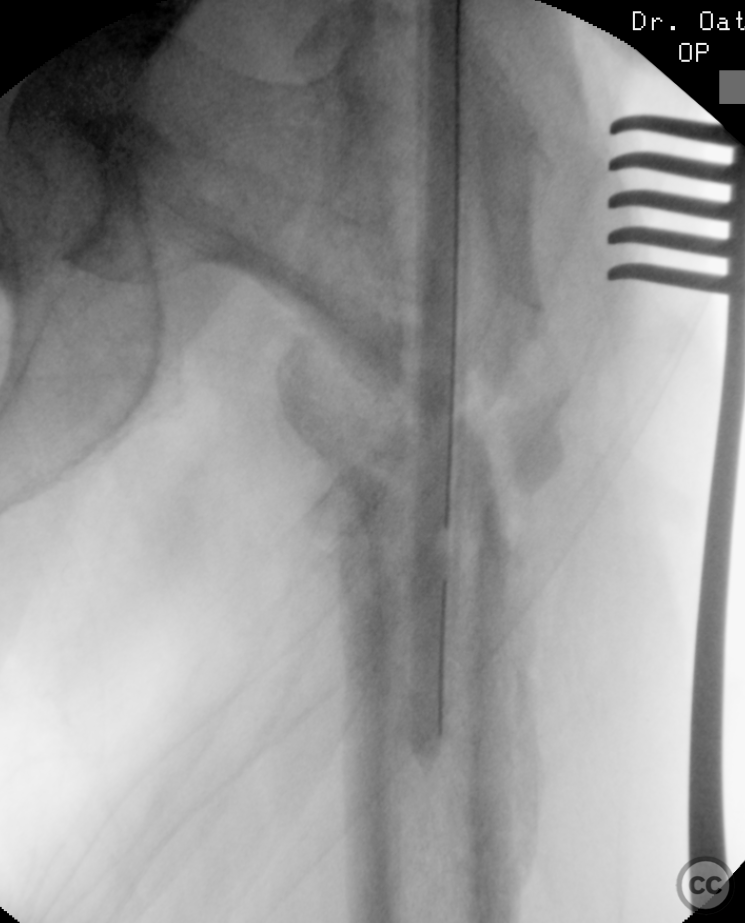
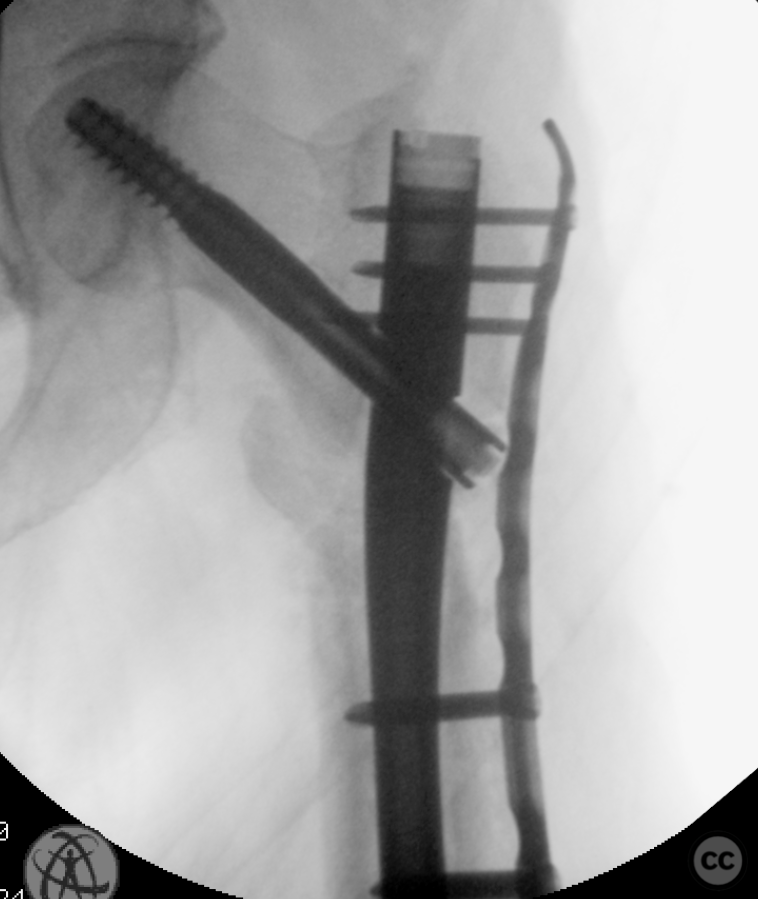
Clinical and radiological findings: A 65-year-old female experienced a low-energy fall resulting in a grossly displaced reverse-cut subtrochanteric left femur fracture. Initial treatment involved open reduction and internal fixation using cerclage cables and a long gamma nail. Postoperative imaging revealed a non-anatomic reduction with varus shift and lateral displacement at the fracture level. Despite these findings, the patient was mobilized under full weight-bearing (FWB) conditions. Three months postoperatively, the patient presented with atraumatic new-onset pain. Imaging and clinical findings indicated nonunion with hardware failure, specifically breakage of the nail at the lag screw interface, accompanied by varus collapse, fluffy callus, and periosteal reaction suggestive of a septic nonunion, despite the absence of significant laboratory markers or clinical history indicative of infection.
Preoperative Plan
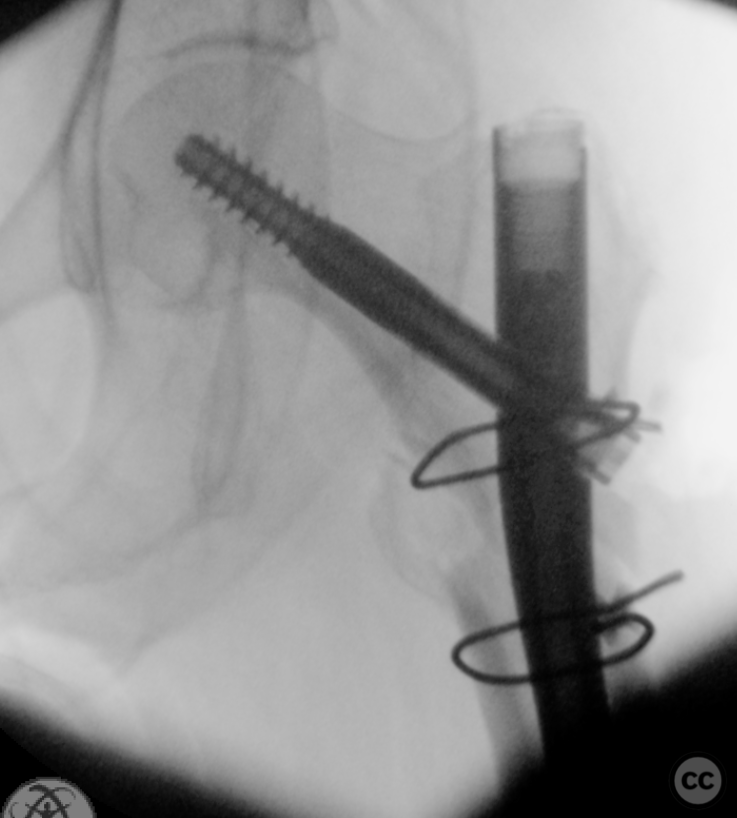
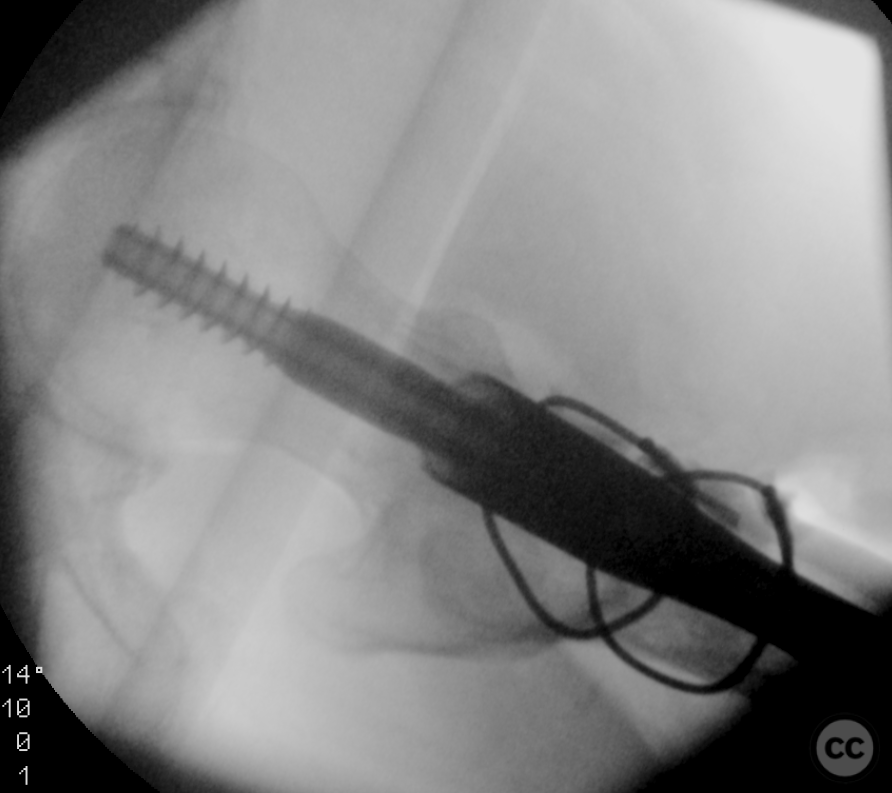
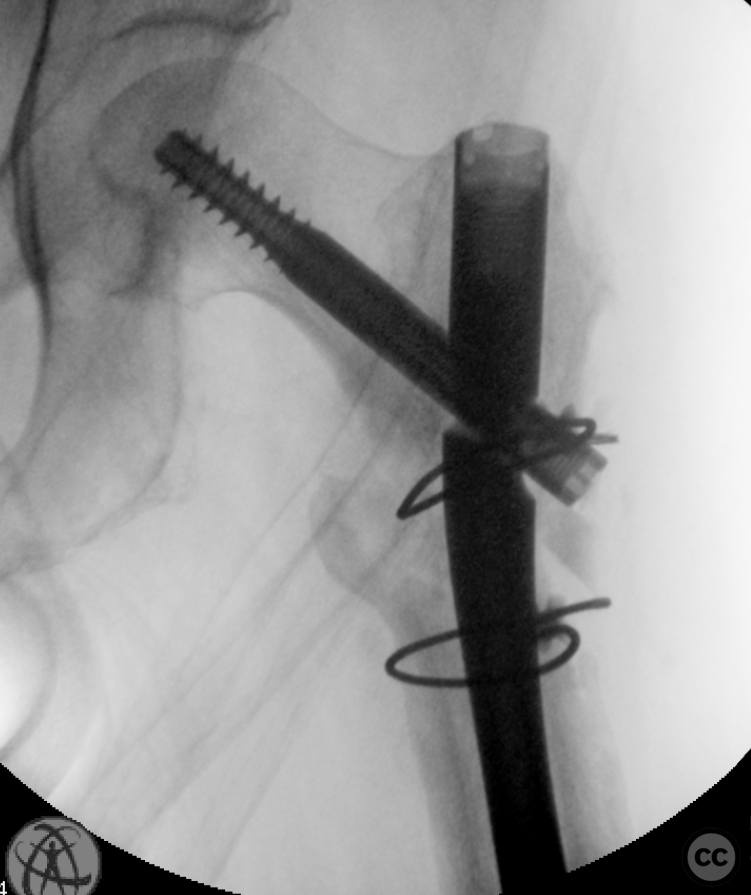
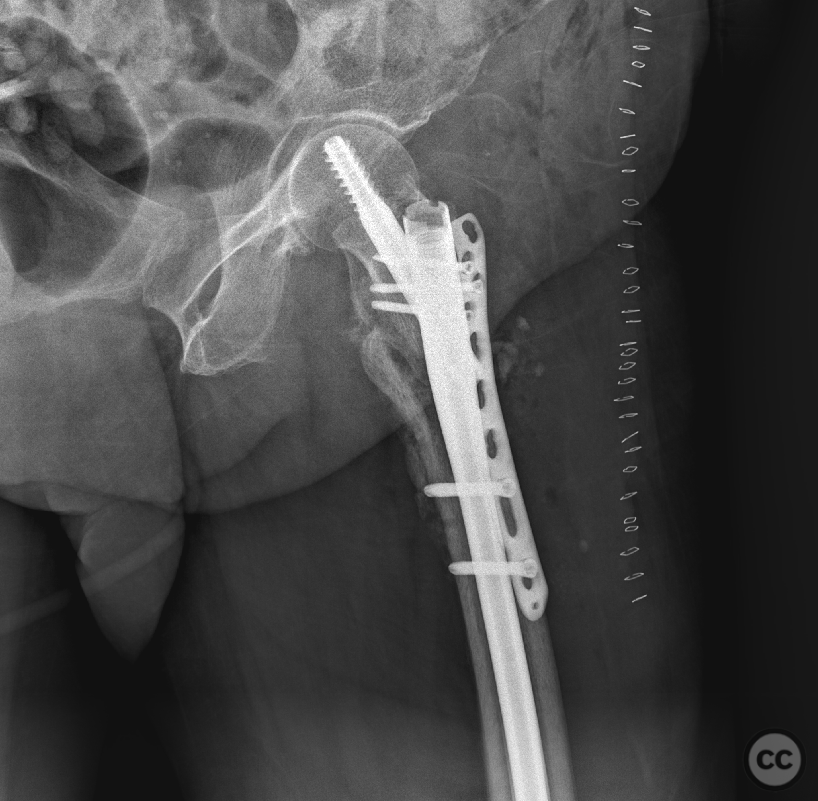
Planning remarks: The preoperative plan involved a single-stage potentially septic revision surgery. The approach would utilize a subvastus appraoch to the proximal femur for hardware removal and debridement of the nonunion site. Reaming of the intramedullary canal and insertion of a revision nail with antibiotic-loaded calcium phosphate were planned, followed by augmentation with a lateral tension/strain-reduction plate.
Surgical Discussion
Patient positioning: The patient was positioned supine on a traction table
Anatomical surgical approach: A subvastus approach to the proximal femur was employed
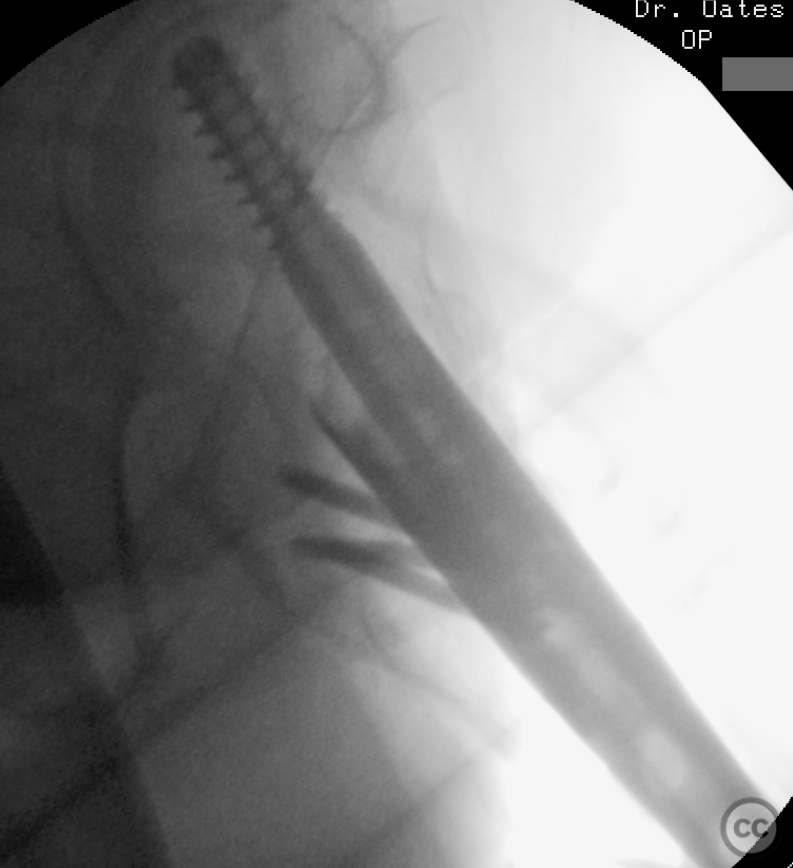
Operative remarks:The initial hardware was unremarkably removed using a "double guidewire" technique for painless removal of the broken distal nail. The intramedullary canal was reamed to 14mm until cortical chatter was achieved. Multiple histological and microbiological samples were taken from the nonunion site to assess for infection. Jet-lavage of the canal followed trial implantation of the revision nail before introducing 30cc of vancomycin/gentamicin-loaded Stimulan in a liquid slurry via a chest tube into the medullary canal. The revision nail was then inserted, and the debrided fracture site was compressed, resulting in approximately 10mm of acute shortening but achieving good bone contact under compression. The procedure was augmented with a lateral tension/strain-reduction plate.
Postoperative protocol: Postoperatively, the patient was mobilized under full weight-bearing conditions to encourage early mobilization and rehabilitation.
Follow up: Not specified
Orthopaedic implants used: Revision intramedullary nail, vancomycin/gentamicin-loaded Stimulan, lateral tension/strain-reduction plate.
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisPlate augmentation has emerged as a viable strategy in cases where initial treatments have failed or when biomechanical considerations necessitate additional stabilization beyond what intramedullary nailing can provide [1-5].
Subtrochanteric fractures are unique due to their anatomical location and the biomechanical forces involved, often resulting in high rates of complications such as malunion, delayed union, and nonunion [4]. Traditional treatment modalities have included both intramedullary nailing and extramedullary fixation with variable outcomes. In instances where these conventional approaches fail to achieve union or when there is significant comminution making stable fixation challenging, plate augmentation has been proposed as an adjunctive technique [2].
Mittal et al.'s study on refractory aseptic subtrochanteric non-unions treated by dual plating highlights the complexity of managing these injuries [3]. Their approach combined proximal femoral locking compression plates (PF-LCP) augmented by lateral compression plates (LCP), alongside biological interventions such as decortication and autologous bone grafting. This method underscores the necessity for both mechanical stability and biological enhancement to facilitate healing in difficult cases.
Similarly, Lo et al. reported on treating subtrochanteric fracture nonunions with intramedullary devices complemented by augmentation side plating [5]. Their findings suggest that this combination not only provides robust mechanical support but also encourages osseous consolidation within an acceptable timeframe without major complications.
Verma et al.'s research into augmentation plating combined with exchange nailing for failed femoral nailing further supports the utility of plate augmentation in addressing complex nonunions [2]. By augmenting existing intramedullary nails with lateral plates, they achieved union across all cases studied, underscoring the effectiveness of combining internal fixation methods to enhance stability.
The literature consistently illustrates that achieving successful outcomes in subtrochanteric fracture nonunions requires careful consideration of both biomechanical stability and biological healing processes. Plate augmentation offers a promising solution by providing supplementary structural support conducive to bone regeneration—especially critical in scenarios where traditional fixation techniques prove inadequate alone.
In conclusion, while each case must be evaluated individually considering patient-specific factors such as bone quality, comorbidities, and prior surgical interventions; plate augmentation presents a valuable tool in the orthopedic surgeon's armamentarium for managing challenging subtrochanteric fracture nonunions. Future research should aim at prospective comparative studies to better delineate its role relative to other established treatment modalities.
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities










User Discussion (1)
Juan Varela
Nice case,Ed Do you think grafting in these cases make a difference?
Biology wasn’t the problem, trust the mechanics - hopefully fixing stability and risk managing the tension side failure will work
Biology is ALWAYS the problem.
Biology is nothing without stability