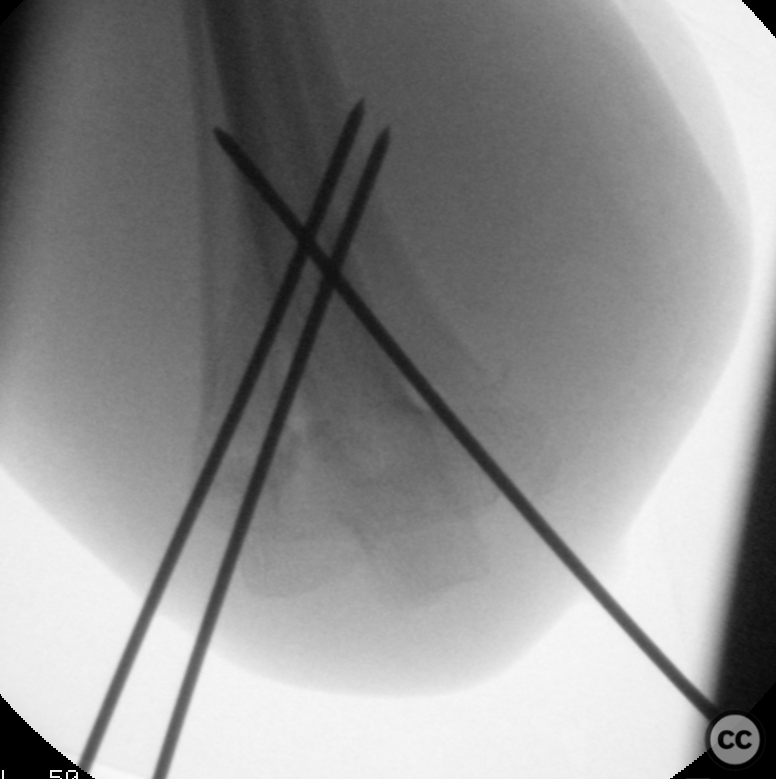
Gartland III-IV SCH fracture - closed reduction and k-wire fixation
Score and Comment on this Case
Clinical Details
Clinical and radiological findings: 7yo patient presents as a helicopter retrieval from a remote location having sustained a right elbow injury in a fall. Patient is heavily sedated and a meaningful nerological exaination is not possible. The injury is closed, there is large eccymosis on the anterior aspect of the elbow joint with puckering of the skin. The hand is pink and warm, cap refill 2sec. Radial pulse is questionably palpable
Preoperative Plan
Planning remarks: For a Gartland IV supracondylar humerus fracture presenting with a pink hand and uncertain neurological status, current literature suggests favoring closed reduction and percutaneous K-wire pinning over open reduction. Despite the inherent challenges of Gartland IV fractures, they can be effectively managed with this technique while avoiding potential complications of open reduction. The preference leans towards crossed pinning due to superior biomechanical stability, which may be particularly pertinent given the inherent instability of Gartland IV fractures. With respect to timing of intervention, even though the optimal timing for a pulseless pink hand scenario is not clearly defined, the questionable neurological status in this case justifies early surgical intervention to prevent potential neurovascular compromise, aligning with the principle of prioritizing nerve integrity over vascular concerns in these fractures.
Surgical Discussion
Patient positioning: Supine with small arm board - see intraop images above.
Anatomical surgical approach: Percutaneous pinning with a samll 6mm open approach medially to allow retraction of the ulnar nerve.
Operative remarks:We grasp the forearm and apply strong longitudinal traction for a minimum of 5-10mins, flexing the elbow to 30deg. Milking manouvers may also be tried in addition to traction. Experiment under fluoroscopy pronating/supinating the forearm to improve alignment of the individual humeral columns. Direct pressure with a thumb on the olecranon can help. It became evident that a posteromedial periosteal hinge was likely assisting stabilisation of the fracture in flexion, resisting the force on the fragment falling into hyeprflexion. After reduction, I tape the elbow in hyperflexion and full pronation. The brachioradialis helped maintain reduction by pulling on the radial humeral column. Two 1.8mm K-wires laterally and one 1.8mm wire medially, protecting the ulnar nerve with a small retractor during medial insertion. Intraoperative fluoroscopy in both hyperfelexed and relaxed positions confirmed stable retention of reduction. Slight oblique views across the lateral projection show reduction of both radial and ulnar columns without rotational malreduction. The hand was pink, cap fill remained 2 sec. pulses poorly palpable, but Allens test demonstrated fast patent flow of both radial and ulnar arteries.
Postoperative protocol: Application of a well-padded, posterior long-arm splint for 3-4 weeks, followed by gentle range-of-motion exercises.
Orthopaedic implants used: Kirschner wires
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisBased on the available evidence, the timing of surgery for pink-and-pulseless supracondylar humerus fractures does not seem to significantly affect the incidence of early postoperative complications or the quality of reduction. One retrospective study by Suganuma et al. (2020) found no significant difference in the incidence of early complications, surgical time, reduction procedure, or radiographic parameters between patients who underwent surgery within 12 hours and those who underwent surgery more than 12 hours after the fracture. Another retrospective study by Abbott et al. (2014) also found no significant correlation between the time to surgery and complications, operative time, or conversion to open reduction. Similarly, a retrospective study by Okkaoglu et al. (2021) concluded that there may not be a time interval within the first 24 hours that makes a difference in terms of early postoperative reduction quality, duration of surgery, or open reduction rate. Furthermore, a study by Mahan et al. (2022) developed a clinical algorithm based on radiographic predictors and clinical characteristics to guide the timing of treatment for completely displaced supracondylar humerus fractures. The algorithm recommended surgery overnight for patients with a "pink pulseless" extremity or motor nerve injury and surgery the next day for patients with a displacement of any cortex by at least 25 mm on radiographs. Additionally, a study by Du et al. (2019) investigated the value of radiologist interpretations in the management of pediatric supracondylar humerus fractures. The study found that radiologist interpretations did not change orthopedic management in any cases. Overall, the available evidence suggests that the timing of surgery for pink-and-pulseless supracondylar humerus fractures may not have a significant impact on outcomes. Further research is needed to validate these findings and to determine the optimal timing for surgical intervention in these fractures.
Author's Resources & References
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant
Industry Sponsership
contact us for advertising opportunities













Article viewed 2371 times
20 Apr 2023
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2023). Gartland III-IV SCH fracture - closed reduction and k-wire fixation. Journal of Orthopaedic Surgery and Traumatology. Case Report 5183048 Published Online Apr 20 2023.