Open posterolateral elbow dislocation with displaced radial neck fracture
Score and Comment on this Case
Clinical Details
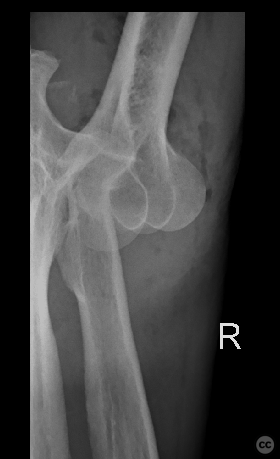
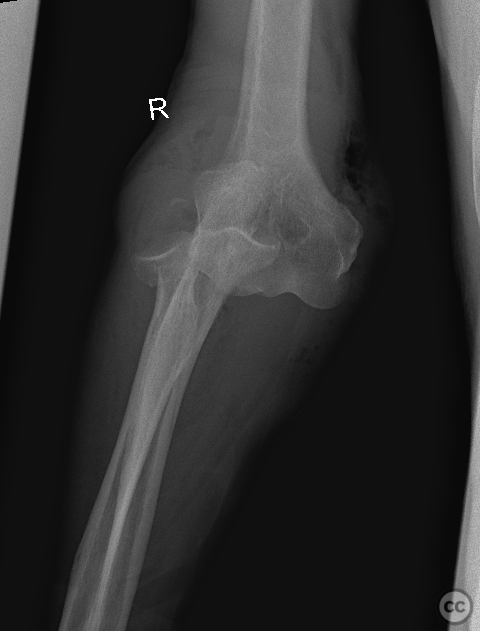
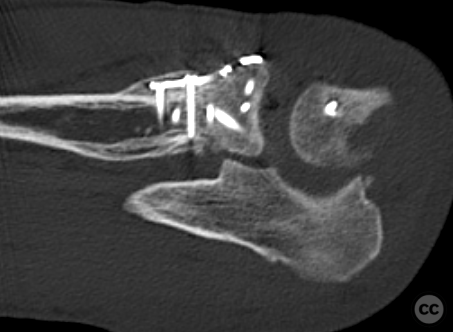
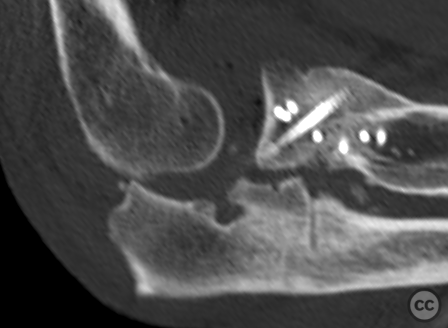
Clinical and radiological findings: A 72-year-old male presented after a domestic fall onto an outstretched arm, resulting in a non-contaminated type I open elbow dislocation with the wound located over the medial epicondyle. Neurovascular examination was intact. Initial radiographs revealed a posterolateral elbow dislocation with an impacted and angulated Mason IV radial neck fracture. Emergency management included surgical debridement, washout, and external fixation due to profound initial instability and both medial and lateral soft tissue disruption. Subsequent CT imaging, although of poor quality, indicated bony avulsion injuries of the humeral-sided medial collateral ligament (MCL) and lateral collateral ligament (LCL) complexes, with the radial head appearing intact but poorly visualized.
Preoperative Plan
Planning remarks: The surgical plan involved preparation for a potential radial head replacement, with open reduction and internal fixation (ORIF) through a dorsal approach (Boyd's interval) being the primary strategy. Medial and lateral ligamentous repair or internal bracing was anticipated due to the observed avulsion injuries and clinical instability.
Surgical Discussion
Patient positioning: The patient was positioned supine with the arm positioned in front of the chest on an arm board, facilitating access to the dorsal aspect of the elbow.
Anatomical surgical approach: The surgical approach utilized was a dorsal approach through Boyd's interval, with reflection of the anconeus muscle down to the supinator ridge. This involved releasing the lateral ulnar collateral ligament (LUCL) to expose the radial head and neck.
Operative remarks:Despite initial concerns, the radial head was found to be intact, but with significant impaction and bone loss on one side of the neck. Given the good bone quality and the large size of the radial head, a decision was made to pursue ORIF rather than replacement. An Aptus radial head rim plate with 2.0mm screws provided monoaxial stability; however, due to the extent of impaction and bony defect, additional stabilization was achieved using 2x HBS screws in a tripod configuration opposite to the plate. This construct ensured excellent reduction stability. The LUCL was reattached with transosseous sutures through the ulna. Subsequently, a subcutaneous flap was elevated to access the EDC split interval where a bony LCL avulsion from the humerus was identified and repaired using a 3.5mm titanium anchor at the isometric point on the capitellum. Both LCL and LUCL were whip-stitched and approximated back to the humeral condyle. Stability assessment under live fluoroscopy through full passive range of motion to full extension revealed no residual instability, with medial gapping on valgus stress deemed inconsequential for functional stability.
Postoperative protocol: Postoperatively, the patient was placed in an elbow orthosis allowing free active/passive range of motion for 8 weeks, with maximum weight-bearing limited to that of a cup of coffee.
Follow up: CT provided is at 9months demonstrating consolidation. Pat presented at this tmie following a new fall sustaining a new open dislocation - hence the imaging
Orthopaedic implants used: Aptus 2.0mm radial head rim plate - 2x HBS screws for tripod stabilization - Arthrex 3.5mm titanium corkscrew anchor
PubMed® Literature Review
Generated by The Literature - Realtime PubMed® AnalysisThe role of medial ligamentous stabilization in elbow dislocation when the radial head is repaired and the joint clinically stable is an intricate aspect of managing complex elbow instability [1-12]. The complexity arises due to the multifactorial nature of elbow stability, which involves bone articulation congruity, capsuloligamentous integrity, and muscle forces.
In cases where there is a fracture-dislocation involving both the radial head repair and coronoid process fixation (as part of "terrible triad" injuries or similar complex patterns), medial collateral ligament (MCL) repair may be necessary if clinical instability persists after lateral collateral ligament (LCL) repair [2][5][7]. This approach aims at restoring varus-valgus stabilizers alongside bony architecture reconstruction.
The MCL's contribution becomes particularly significant when addressing posteromedial rotatory instability—a condition often underappreciated but increasingly recognized as a critical component in complex elbow dislocations [8]. When associated with anteromedial facet fractures of the coronoid process along with LCL disruption resulting from varus posteromedial forces, MCL reconstruction can be pivotal for achieving joint stability [9].
Moreover, intraoperative assessment under fluoroscopy after radial head fixation/replacement reveals that some elbows remain unstable despite seemingly adequate osseous repairs. In these instances, direct repair or even reconstruction using tendon grafts for the MCL has been advocated by several authors [4][6][10]. It should be noted that persistent instability following LCL repair necessitates consideration for additional medial side intervention—either through direct repair or hinged external fixator application—if early mobilization within a stable arc is desired [3].
It's also important to highlight that while lateral-sided injuries are more common due to typical injury mechanisms leading to elbow dislocations with associated radial head fractures; however, neglecting potential damage on the medial side can lead to suboptimal outcomes such as recurrent instability or chronic valgus overload states leading eventually to arthritic changes [11].
The literature suggests that successful outcomes depend on achieving concentric reduction and maintaining it throughout early motion exercises postoperatively. This goal often requires meticulous attention not only to bony anatomy restoration but also careful evaluation—and subsequent treatment—of soft tissue structures including both collateral ligaments [12].
In summary, medial ligamental stabilization plays an adjunctive yet crucial role in certain cases where clinical stability cannot be achieved solely by addressing lateral column injuries alongside radial head repairs. The decision-making must be individualized based on intraoperative findings following initial osseous reconstructions coupled with dynamic testing for residual laxity or instability patterns
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities










Article viewed 1249 times
07 Feb 2024
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2024). Open posterolateral elbow dislocation with displaced radial neck fracture. Journal of Orthopaedic Surgery and Traumatology. Case Report 6248788 Published Online Feb 07 2024.