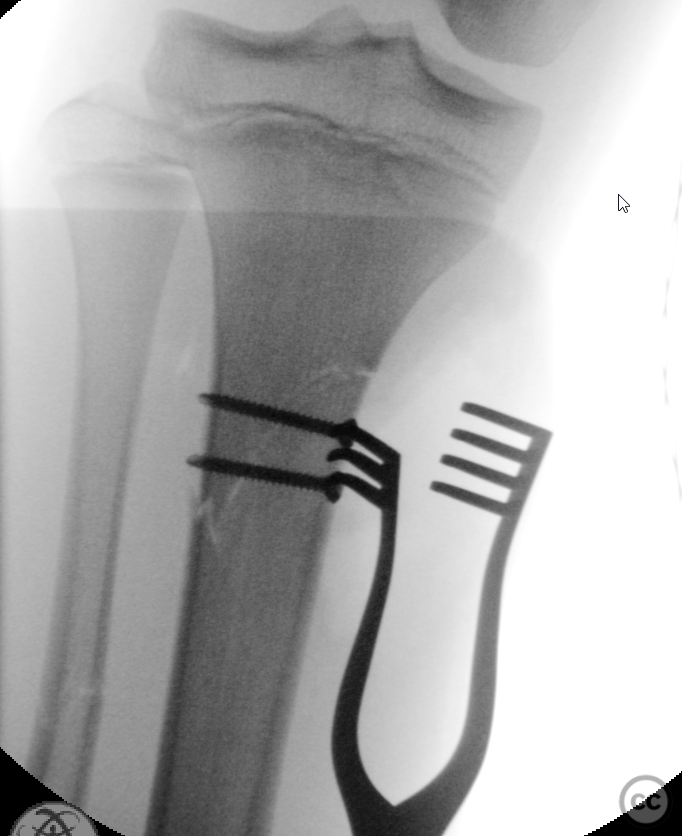
13yo proximal tibial diametaphyseal transition zone fracture
Score and Comment on this Case
Clinical Details
Clinical and radiological findings: A relatively high energy sports injury sustained by a 13yo M. Closed and NV intact. Isolated limb trauma. Significant swelling without clinical suspicion of compartment development. Initial management in ED including reduction and splinting under procedural sedation demonstrated an intact lateral periosteal hinge and soft tissue block / interposition medially. Axial alignment tended to slight values, though this is poorly shown on provided imaging.
Preoperative Plan
Planning remarks: Plan was attempt MUA and formal closed reduction. MUA demonstrated persistent interposition medially and which failed to achieve anatomic closed reduction. Institutional policy is to not accept malreduced axis deviation if a procedure has already escalated to management in operating theatres. Progression to ORIF was therefore indicated following failure of closed reduction.
Surgical Discussion
Patient positioning: Supine
Anatomical surgical approach: Limited anteromedial longitudinal approach over the fracture curving slightly posteriorly over pes. Incision ~7cm
Operative remarks:Location of the fracture was immediately distal to the pes insertion suggesting the external valgus forced had loaded against an adduction / varus constraint provided by both the MCL and hamstrings. Both the distal aspect of the superficial MCL together with distal fibres of pes and periosteum were incarcerated in the fracture preventing reduction. Removal of interposition facilitated correction of the slight rotational deformity, together with correction of valgus. The fracture was lagged ML with 2 3.5mm cortical screws, then neutralised with a 3.5mm LCP locking plate. The plate was pre contoured to not actively influence the now anatomically restored native long axis. The plate was placed anterior to pes as posterior placement under the hamstrings would have been off-axis to counter any valgus collapse. The most proximal screw was kept monocortical below the level of the physis. The MCL was considered clinically stable. No adjuvant fixation of MCL was done
Postoperative protocol: No splint during the day, and TWB for 4 weeks. PWB from week 5 progressing to FWB by week 6 post.
Orthopaedic implants used: 3.5mm Synthes LCP locking plate
Search for Related Literature

Dr Ed Oates
- Germany , Schleswig Holstein
- Area of Specialty - General Trauma
- Position - Specialist Consultant

Industry Sponsership
contact us for advertising opportunities






Article viewed 3719 times
14 Feb 2023
Add to Bookmarks
Full Citation
Cite this article:
Oates, E.J. (2023). 13yo proximal tibial diametaphyseal transition zone fracture. Journal of Orthopaedic Surgery and Traumatology. Case Report 9061389 Published Online Feb 14 2023.